Andy
Senior Member (Voting rights)
Full title: Numbers and types of neurological emergencies in England and the influence of socioeconomic deprivation: a retrospective analysis of hospital episode statistics data
Abstract
Objectives
In this first large-scale analysis of neurological emergency admissions in England, we determine the number and types of emergency admissions with neurological emergency diagnostic codes, how many are under the care of a neurologist or neurosurgeon and how such admissions vary by levels of deprivation.
Design
Retrospective empirical research employing a derived list of neurological emergency diagnostic codes
Setting
This study used the Hospital Episode Statistics data set for the financial year 2019/2020 based on 17 million in-year inpatient admissions in England including 6.5 million (100%) emergency admissions with any diagnosis codes.
Results
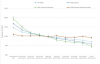
There were 1.4 million (21.2%) emergency inpatient admissions with a mention of any neurological code, approx. 248 455 (3.8%) with mention of a specific neurological emergency code from the derived list, and 72 485 (1.1%) included such a code as the primary reason for admission. The highest number of in-year admissions for adults was for epilepsy (145 995), with epilepsy as the primary diagnostic code in 15 945 (10.9%). Acute nerve root/spinal cord syndrome (41 215), head injury (29 235) and subarachnoid haemorrhage (18 505) accounted for the next three highest number of admissions. 3230 (1.4%) in-year emergency hospital admissions with mention of a neurological emergency code were under the care of a neurologist or neurosurgeon, with only 1315 (0.9%) admissions with mention of an epilepsy code under a neurologist. There was significant variation for epilepsy and functional neurological disorders (FNDs) in particular by Index of Multiple Deprivation decile. The association between deprivation and epilepsy and FND was significant with p-values of 2.5e-6 and 1.5e-8, respectively.
Conclusions
This study has identified important findings in relation to the burden of neurological emergency admissions but further work is needed, with greater clinical engagement in diagnostic coding, to better understand the implications for workforce and changes to service delivery needing to be implemented.
Open access, https://bmjopen.bmj.com/content/12/11/e061843#DC1
Abstract
Objectives
In this first large-scale analysis of neurological emergency admissions in England, we determine the number and types of emergency admissions with neurological emergency diagnostic codes, how many are under the care of a neurologist or neurosurgeon and how such admissions vary by levels of deprivation.
Design
Retrospective empirical research employing a derived list of neurological emergency diagnostic codes
Setting
This study used the Hospital Episode Statistics data set for the financial year 2019/2020 based on 17 million in-year inpatient admissions in England including 6.5 million (100%) emergency admissions with any diagnosis codes.
Results
There were 1.4 million (21.2%) emergency inpatient admissions with a mention of any neurological code, approx. 248 455 (3.8%) with mention of a specific neurological emergency code from the derived list, and 72 485 (1.1%) included such a code as the primary reason for admission. The highest number of in-year admissions for adults was for epilepsy (145 995), with epilepsy as the primary diagnostic code in 15 945 (10.9%). Acute nerve root/spinal cord syndrome (41 215), head injury (29 235) and subarachnoid haemorrhage (18 505) accounted for the next three highest number of admissions. 3230 (1.4%) in-year emergency hospital admissions with mention of a neurological emergency code were under the care of a neurologist or neurosurgeon, with only 1315 (0.9%) admissions with mention of an epilepsy code under a neurologist. There was significant variation for epilepsy and functional neurological disorders (FNDs) in particular by Index of Multiple Deprivation decile. The association between deprivation and epilepsy and FND was significant with p-values of 2.5e-6 and 1.5e-8, respectively.
Conclusions
This study has identified important findings in relation to the burden of neurological emergency admissions but further work is needed, with greater clinical engagement in diagnostic coding, to better understand the implications for workforce and changes to service delivery needing to be implemented.
Open access, https://bmjopen.bmj.com/content/12/11/e061843#DC1