Not sure whether this tells us much about ME/CFS and similar given:
“What was surprising was that, for both groups, heart rate and step count eventually returned to pre-infection levels,” Ledebur notes. “Despite ongoing shortness of breath and/or fatigue, affected individuals took as many steps as they did before infection,” says Ledebur.
-----
https://www.eurekalert.org/news-releases/1077453
News Release 20-Mar-2025
Smartwatch data: Study finds early health differences in long COVID patients
People who later experienced persistent shortness of breath or fatigue after a SARS-CoV-2 infection were already taking significantly fewer steps per day and had a higher resting heart rate before contracting the virus, according to a CSH study
Peer-Reviewed Publication
Complexity Science Hub
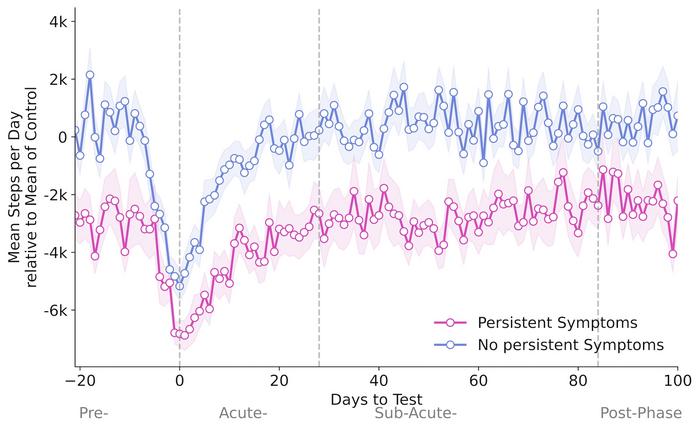
image:
Mean resting heart rate (top) and mean daily steps relative to the average of individuals with Covid-19 infection but without persistent symptoms (bottom) before, during, and after a Covid-19 infection. The pink line represents patients who developed persistent symptoms, while the blue line represents those who did not.
view more
Credit: Complexity Science Hub
[Vienna, 19.03.2025]—Between April 2020 and December 2022, over 535,000 people in Germany downloaded and activated the Corona Data Donation App (CDA). Of these, more than 120,000 voluntarily shared daily data from their smartwatches and fitness trackers with researchers, providing insights into vital functions such as resting heart rate and step count.
“These high-resolution data served as the starting point for our study,” explains
CSH researcher
Katharina Ledebur. “We were able to compare vital signs in 15-minute intervals before, during, and after a SARS-CoV-2 infection.”
Higher Resting Heart Rate And 3,000 Fewer Steps
People with persistent symptoms showed significant differences in activity levels and resting heart rate compared to others. “In the three weeks before infection, patients who later reported persistent symptoms took an average of just 5,075 steps per day—about 3,030 fewer than SARS-CoV-2 patients who recovered without persistent symptoms,” says Ledebur.
Resting heart rates also showed differences before infection. Those who later developed persistent symptoms had a resting heart rate 2.37 beats per minute higher than individuals who recovered without lingering effects. Additionally, they exhibited a more pronounced and prolonged phase of slowed resting heart rate—known as bradycardia—lasting up to 18 days after infection.
“What was surprising was that, for both groups, heart rate and step count eventually returned to pre-infection levels,” Ledebur notes. “Despite ongoing shortness of breath and/or fatigue, affected individuals took as many steps as they did before infection,” says Ledebur.
Two Persistent Symptoms
For the study, researchers divided smartwatch and fitness tracker data into four phases: before infection, during the acute infection (0 to 4 weeks after a positive test), the subacute phase (5 to 12 weeks after a positive test), and the post-acute phase (beyond 12 weeks).
Participants also completed monthly and weekly surveys about Covid-19 tests, their subjective well-being, and ongoing symptoms.
“Using these symptom reports, we found that among 11 symptoms analyzed, only shortness of breath and fatigue persisted beyond the acute phase of SARS-CoV-2 infection. Other symptoms, such as cough, headache, or fever, showed no long-term effects,” Ledebur explains.
Overall, 2.6% of all SARS-CoV-2-positive individuals reported prolonged shortness of breath, 10.4% experienced long-lasting fatigue, and 1.8% had both symptoms.
Raising Awareness And Protecting At-Risk Individuals
The findings of this study suggest that persistent symptoms may be linked to lower fitness levels or preexisting health conditions.
“However, this does not mean that a higher resting heart rate, lower step count, or preexisting conditions alone are responsible for these symptoms,” Ledebur emphasizes. “Rather, they highlight the need for special attention and protective measures for affected individuals,” says Ledebur, who is also a PhD candidate at the Medical University of Vienna.
Exceptional Data Quality
Thanks to the high-resolution smartwatch data from the Corona Data Donation App (CDA), researchers were able to compare not only different patients but also individual changes over time. “If you examine people after they have been infected, you cannot assess individual changes because you lack baseline information,” explains
Peter Klimek from CSH and the Medical University of Vienna.
“Despite the advantages of such data, there are limitations: Men are overrepresented, while both adolescents and individuals over 65—who have a higher risk—are underrepresented,” Ledebur notes. Additionally, people who wear smartwatches or fitness trackers may generally be more health-conscious.
“Nevertheless, the study highlights the enormous potential of smartwatches to provide valuable, objective insights into the physiological and behavioral effects of an infection and to help identify individuals at higher risk,” the researchers conclude.
The CDA was launched by the Robert Koch Institute under the leadership of
Dirk Brockmann, CSH external faculty member and professor at TU Dresden.
About the study
The study “Wearable Data Reveals Distinct Characteristics of Individuals with Persistent Symptoms after a SARS-CoV-2 Infection” by
K. Ledebur, M. Wiedermann, C. Puta,
S. Thurner,
P. Klimek, and
D. Brockmann was published in
npj Digital Medicine (doi: 10.1038/s41746-025-01456-x).
About CSH
The
Complexity Science Hub (CSH) is Europe’s research center for the study of complex systems. We derive meaning from data from a range of disciplines—economics, medicine, ecology, and the social sciences—as a basis for actionable solutions for a better world. Established in 2015, we have grown to over 70 researchers, driven by the increasing demand to gain a genuine understanding of the networks that underlie society, from healthcare to supply chains. Through our complexity science approaches linking physics, mathematics, and computational modeling with data and network science, we develop the capacity to address today’s and tomorrow’s challenges.
Journal
npj Digital Medicine
DOI
10.1038/s41746-025-01456-x
Method of Research
Data/statistical analysis
Subject of Research
People
Article Title
Wearable data reveals distinct characteristics of individuals with persistent symptoms after a SARS-CoV-2 infection
Article Publication Date
19-Mar-2025
COI Statement
The authors declare no competing interests.
Disclaimer: AAAS and EurekAlert! are not re

