InitialConditions
Senior Member (Voting Rights)
Postural orthostatic tachycardia syndrome (POTS) is a chronic, multifactorial syndrome with complex symptoms of orthostatic intolerance. Breathlessness is a prevalent symptom, however little is known about the aetiology. Anecdotal evidence suggests that breathless POTS patients commonly demonstrate dysfunctional breathing/hyperventilation syndrome (DB/HVS). There are, however, no published data regarding DB/HVS in POTS, and whether physiotherapy/breathing retraining may improve patients' breathing pattern and symptoms.
The aim of this study was to explore the potential impact of a physiotherapy intervention involving education and breathing control on DB/HVS in POTS. A retrospective observational cohort study of all patients with POTS referred to respiratory physiotherapy for treatment of DB/HVS over a 20-month period was undertaken.
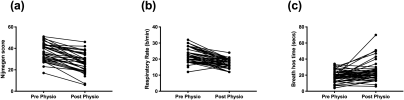
100 patients (99 female, mean (standard deviation) age 31 (12) years) with a clinical diagnosis of DB/HV were referred, of which data was available for 66 patients pre – post intervention. Significant improvements in Nijmegen score, respiratory rate and breath hold time (seconds) were observed following treatment. These data provide a testable hypothesis that breathing retraining may provide breathless POTS patients with some symptomatic relief, thus improving their health-related quality of life. The intervention can be easily protocolised to ensure treatment fidelity. Our preliminary findings provide a platform for a subsequent randomised controlled trial of breathing retraining in POTS.
LINK
The aim of this study was to explore the potential impact of a physiotherapy intervention involving education and breathing control on DB/HVS in POTS. A retrospective observational cohort study of all patients with POTS referred to respiratory physiotherapy for treatment of DB/HVS over a 20-month period was undertaken.
100 patients (99 female, mean (standard deviation) age 31 (12) years) with a clinical diagnosis of DB/HV were referred, of which data was available for 66 patients pre – post intervention. Significant improvements in Nijmegen score, respiratory rate and breath hold time (seconds) were observed following treatment. These data provide a testable hypothesis that breathing retraining may provide breathless POTS patients with some symptomatic relief, thus improving their health-related quality of life. The intervention can be easily protocolised to ensure treatment fidelity. Our preliminary findings provide a platform for a subsequent randomised controlled trial of breathing retraining in POTS.
LINK