Sly Saint
Senior Member (Voting Rights)
 Charles C. Edwards III1 Charles C. Edwards II2 Scott Heinlein3
Charles C. Edwards III1 Charles C. Edwards II2 Scott Heinlein3  Peter C. Rowe4*
Peter C. Rowe4*Introduction:
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a complex, chronic, multi-system disorder that is characterized by a substantial impairment in the activities that were well tolerated before the illness. In an earlier report, we had described three adult women who met criteria for ME/CFS and orthostatic intolerance, and had congenital or acquired cervical spinal stenosis. All three experienced substantial global improvements in their ME/CFS and orthostatic intolerance symptoms after recognition and surgical treatment of the cervical stenosis. After a several year period of improvement, one of the individuals in that series experienced a return of ME/CFS and orthostatic intolerance symptoms.
Main Symptoms and Clinical Findings:
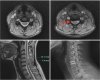
Radiologic investigation confirmed a recurrence of the ventral compression of the spinal cord due to a shift of the disc replacement implant at the involved cervical spinal level.
Therapeutic Intervention:
Decompression of the spinal cord with removal of the implant and fusion at the original C5-C6 level was once again followed by a similar degree of improvement in function as had been observed after the first operation.This recapitulation of the outcomes after surgical management of cervical stenosis provides further evidence in support of the hypothesis that cervical spinal stenosis can exacerbate pre-existing or cause new orthostatic intolerance and ME/CFS. Especially for those with refractory symptoms and neurological signs, surgical interventions may offer relief for selected patients with this complex condition.
https://www.frontiersin.org/articles/10.3389/fneur.2023.1284062/abstract