Andy
Senior Member (Voting rights)
The COVID-19 pandemic taught us many lessons, including the interconnection between physical and mental health. This observation is not new, however; the intersection of physical and mental health is discussed in early medical writings. At the origins of modern-day psychiatry and neurology, there was great interest in the condition now called functional neurological disorder (FND) (1, 2). Nonetheless, FND has a complex history, including its evolution from “hysteria” to “conversion” to “psychogenic illness” to “FND”; unfortunately, the condition is also stigmatized and erroneously confused with malingering (3). The recognition that FND is common, an emphasis on a rule-in diagnosis, an improved understanding of mechanisms and etiologies, and an expanding therapeutic toolkit have revitalized the field of FND (4). However, disagreements remain, such as the multiplicity of terms used for the seizure subtype of FND (e.g., psychogenic nonepileptic vs. functional vs. dissociative vs. nonepileptic attacks) (5); to unambiguously connect all functional neurological subtypes to FND, we support use of the term “functional seizures.”
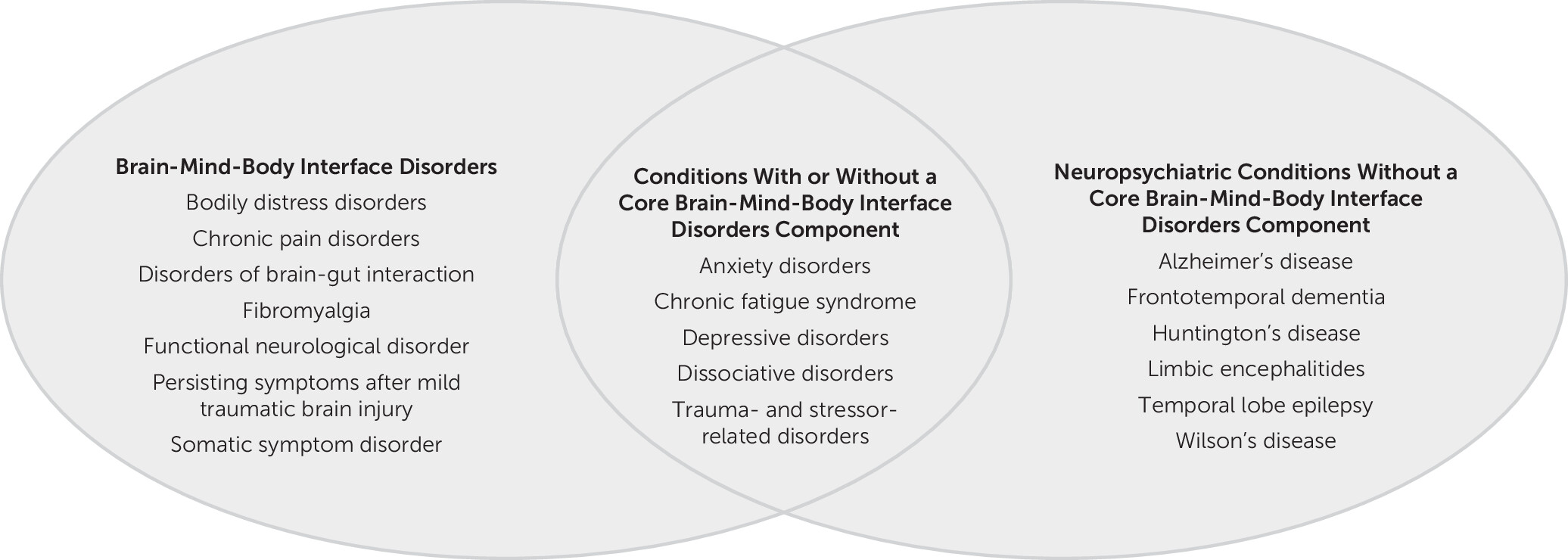
In other specialties, similar transformations have moved away from “medically unexplained” framings. Although certain disciplines have used the qualifier “functional” and this term is well received by some patients and advocacy groups, challenges to a “functional disorders” diagnostic category remain (6). The term “functional gastrointestinal disorders” was changed to “disorders of gut-brain interaction,” in part because “functional” was thought to be too nonspecific (7). The somatic symptom disorder diagnosis has received mixed reviews, and competing terms, such as bodily distress disorders, have arisen (8). These developments have weakened the DSM-5’s “Somatic Symptom and Related Disorders” category. In parallel, the medical literature has codified functional somatic syndromes (e.g., fibromyalgia) with their own diagnostic criteria. Some conditions have been reframed to potentially distance them from a biopsychosocial-informed therapeutic framework (e.g., myalgic encephalomyelitis or chronic fatigue syndrome); conversely, there have been calls to reconceptualize persistent symptoms after traumatic brain injury (also known as postconcussive symptoms or postconcussion syndrome) as an “interface disorder of neurology, psychiatry, and psychology” (9).
Here, we make the case for a “brain-mind-body interface disorders” diagnostic category spanning medical specialties; this category represents conditions with physical symptoms where there is likely a therapeutic benefit to factor in psychological processes.
Open access, https://neuro.psychiatryonline.org/doi/10.1176/appi.neuropsych.20230071
In other specialties, similar transformations have moved away from “medically unexplained” framings. Although certain disciplines have used the qualifier “functional” and this term is well received by some patients and advocacy groups, challenges to a “functional disorders” diagnostic category remain (6). The term “functional gastrointestinal disorders” was changed to “disorders of gut-brain interaction,” in part because “functional” was thought to be too nonspecific (7). The somatic symptom disorder diagnosis has received mixed reviews, and competing terms, such as bodily distress disorders, have arisen (8). These developments have weakened the DSM-5’s “Somatic Symptom and Related Disorders” category. In parallel, the medical literature has codified functional somatic syndromes (e.g., fibromyalgia) with their own diagnostic criteria. Some conditions have been reframed to potentially distance them from a biopsychosocial-informed therapeutic framework (e.g., myalgic encephalomyelitis or chronic fatigue syndrome); conversely, there have been calls to reconceptualize persistent symptoms after traumatic brain injury (also known as postconcussive symptoms or postconcussion syndrome) as an “interface disorder of neurology, psychiatry, and psychology” (9).
Here, we make the case for a “brain-mind-body interface disorders” diagnostic category spanning medical specialties; this category represents conditions with physical symptoms where there is likely a therapeutic benefit to factor in psychological processes.
Open access, https://neuro.psychiatryonline.org/doi/10.1176/appi.neuropsych.20230071