Dx Revision Watch
Senior Member (Voting Rights)
Welcome to the forum, @cfsandmore
And they are likely to continue to do so until science sorts out aetiology and subsets.
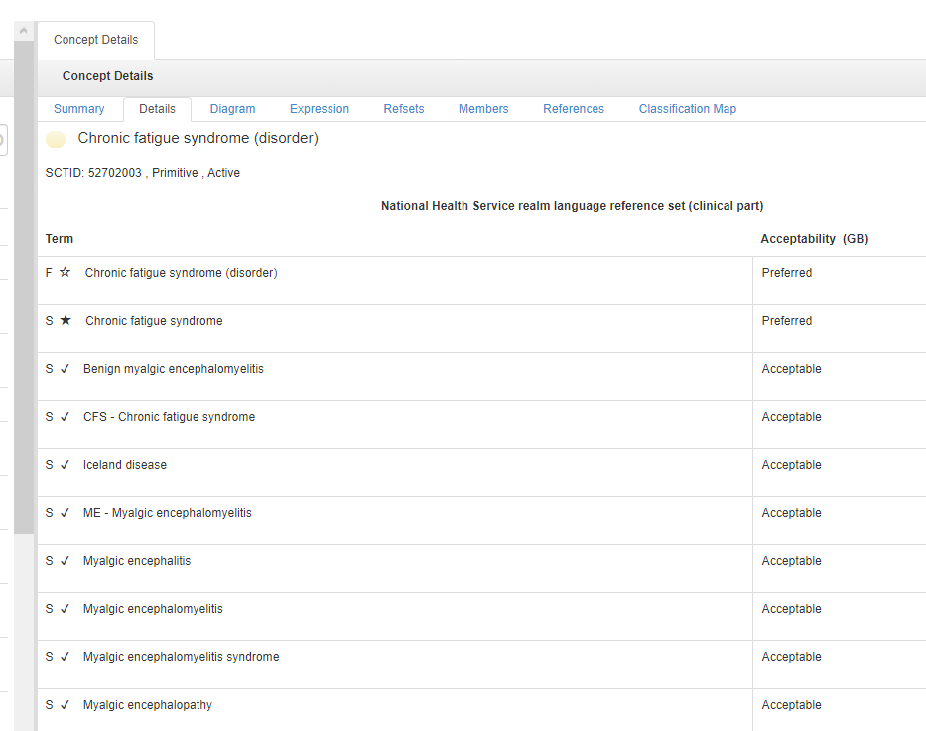
The International Edition of SNOMED CT terminology system and the various national extensions all have Chronic fatigue syndrome listed as the "Preferred" Concept term, with a number of alternative terms under Synonyms (including Myalgic encephalomelitis) listed as "Acceptable" (all terms have been cross mapped to ICD-10's G93.3).
Germany's ICD-10-GM has "Chronisches Müdigkeitssyndrom [Chronic fatigue syndrome]" as the G93.3 Concept Title term – not Postviral fatigue syndrome. The US's ICD-10-CM has a choice of selecting one of two codes: R53.82 or G93.3, depending on whether, in the clinician's judgement, there is enough evidence to attribute the patient's illness to a viral onset [1].
1 Source: ICD-related questions from CFSAC's May 2011 meeting, background document presented by Dr Wanda Jones to the CFSAC Committee:
Dr Jones further clarified for the Committee that:
It was further confirmed, shortly after that meeting, that testing for a viral illness is not required to assign a code – that coding is based on the clinician's judgement.
Source: NCHS/CDC September 14, 2011 Coordination and Maintenance Committee Meeting, Diagnosis Agenda Proposals document:
Many patients in the US will have been diagnosed using the R53.82 Chronic fatigue syndrome NOS code.
It is not known what percentage of newly diagnosed patients in the US have been assigned the G93.3 code rather than the R53.82 code since October 2015, when ICD-10-CM was finally implemented for morbidity use for records and reimbursement.
Before publicly promoting any proposals for how terms might potentially be used going forward (whether in the context of ME, CFS patients or patients with chronic post COVID-19 symptoms), a thorough understanding of how diagnostic terms are currently recorded in patient electronic medical records (EMRs) using SNOMED CT and reported for reimbursement and statistical analysis using ICD-10 or national modifications of ICD-10 is essential.
For example, the US's R53.82 Chronic fatigue syndrome NOS code is intended for use when the physician has not established a link with a past viral infection.
But Dr O'Leary writes:
[Edited for clarity]
...As others have explained CFS is a name often used by Primary Care Physicians and General Practitioners, my doctor still uses CFS.
And they are likely to continue to do so until science sorts out aetiology and subsets.
The International Edition of SNOMED CT terminology system and the various national extensions all have Chronic fatigue syndrome listed as the "Preferred" Concept term, with a number of alternative terms under Synonyms (including Myalgic encephalomelitis) listed as "Acceptable" (all terms have been cross mapped to ICD-10's G93.3).
Germany's ICD-10-GM has "Chronisches Müdigkeitssyndrom [Chronic fatigue syndrome]" as the G93.3 Concept Title term – not Postviral fatigue syndrome. The US's ICD-10-CM has a choice of selecting one of two codes: R53.82 or G93.3, depending on whether, in the clinician's judgement, there is enough evidence to attribute the patient's illness to a viral onset [1].
1 Source: ICD-related questions from CFSAC's May 2011 meeting, background document presented by Dr Wanda Jones to the CFSAC Committee:
"As it relates to CFS the use of two codes is consistent with the classification as there would be a code to capture CFS when the physician has determined the cause as being due to a past viral infection (G93.3) or if the physician has not established a link with a past viral infection (R53.82).
If code R53.82 were eliminated it would not be possible to disaggregate cases that are now distinguishable through the use of two codes.
There is a general equivalence map between ICD-9-CM and ICD-10-CM codes, however, if a concept is not carried over from the earlier version to the newer version data will be lost going forward."
If code R53.82 were eliminated it would not be possible to disaggregate cases that are now distinguishable through the use of two codes.
There is a general equivalence map between ICD-9-CM and ICD-10-CM codes, however, if a concept is not carried over from the earlier version to the newer version data will be lost going forward."
Dr Jones further clarified for the Committee that:
"...if however [the clinician] could not identify where the trajectory developed toward CFS, then it would wind up in the R codes."
It was further confirmed, shortly after that meeting, that testing for a viral illness is not required to assign a code – that coding is based on the clinician's judgement.
Source: NCHS/CDC September 14, 2011 Coordination and Maintenance Committee Meeting, Diagnosis Agenda Proposals document:
"In ICD-10-CM chronic fatigue syndrome NOS (that is not specified as being due to a past viral infection) was added to ICD-10-CM in Chapter 18 at R53.82, Chronic fatigue, unspecified. ICD-10-CM retained code G93.3 to allow the differentiation of cases of fatigue syndrome where the physician has determined the cause as being due to a past viral infection from cases where the physician has not established a post viral link. It should be noted that including chronic fatigue syndrome NOS at code G93.3 would make it difficult to disaggregate cases that are now distinguishable through the use of two separate codes."
Many patients in the US will have been diagnosed using the R53.82 Chronic fatigue syndrome NOS code.
It is not known what percentage of newly diagnosed patients in the US have been assigned the G93.3 code rather than the R53.82 code since October 2015, when ICD-10-CM was finally implemented for morbidity use for records and reimbursement.
Before publicly promoting any proposals for how terms might potentially be used going forward (whether in the context of ME, CFS patients or patients with chronic post COVID-19 symptoms), a thorough understanding of how diagnostic terms are currently recorded in patient electronic medical records (EMRs) using SNOMED CT and reported for reimbursement and statistical analysis using ICD-10 or national modifications of ICD-10 is essential.
For example, the US's R53.82 Chronic fatigue syndrome NOS code is intended for use when the physician has not established a link with a past viral infection.
But Dr O'Leary writes:
"When researchers and clinicians tie long Covid to CFS, they can reassure the public that nonspecific long Covid will be resolved through virus recovery strategies."
[Edited for clarity]
Last edited: