Dolphin
Senior Member (Voting Rights)
Tate WP, Peppercorn K, Bowden N, Charlton F. Managing chronic fatigue conditions with overlapping symptoms, and the health policies and social services supporting those affected.
Med Res Arch. 2025 Dec 1;13(11).
https://esmed.org/MRA/mra/article/view/7104
https://esmed.org/MRA/mra/article/view/7104/99193549742
The chronic fatigue conditions, Myalgic Encephalomyelitis/Chronic fatigue syndrome, Long COVID, Fibromyalgia, Ehlers-Danlos syndromes and Multiple sclerosis, share many overlapping symptoms that reflect similar physiological responses, sometimes leading to misdiagnosis, yet the conditions are distinct and are being managed as separate diseases.
The characteristics of what is known about each condition is described here, and as well for two co-morbidities, Postural Orthostatic Tachycardia Syndrome and Mast cell Activation Syndrome intimately linked to the physiological dysfunctions of the chronic conditions.
The pathophysiological changes in immunological function, neurological regulation, metabolism and energy production, and the microbiome affecting the gut-immune brain axis are discussed and compared for each condition.
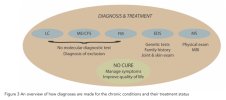
The difficulties encountered for diagnosis, and the current lack of effective treatment option are highlighted.
Evidence is presented that affected patients have pressing needs, and that there are currently barriers that prevent access to more effective health support, result in patients being isolated lifelong from employment, and that block access to the essential social services.
Effective public health policy is needed to ensure these inadequacies in public health support are overcome, and financial support is provided to ensure all patients have an enhanced quality of life.
There may be significant benefit for affected patients if research and collective knowledge of these conditions and comorbidities are shared and more integrated, to promote better understanding for their management, provide a wider range of common treatment options, and stimulate more co-ordinated health policies for the management of patient support.
Multiple sclerosis is far better served than the other conditions and could provide the model for how chronic conditions could be managed better.
Med Res Arch. 2025 Dec 1;13(11).
https://esmed.org/MRA/mra/article/view/7104
https://esmed.org/MRA/mra/article/view/7104/99193549742
Abstract
Complex chronic conditions present a formidable challenge to clinicians to diagnose and manage for their patients, and the diseases are still relatively poorly understood.The chronic fatigue conditions, Myalgic Encephalomyelitis/Chronic fatigue syndrome, Long COVID, Fibromyalgia, Ehlers-Danlos syndromes and Multiple sclerosis, share many overlapping symptoms that reflect similar physiological responses, sometimes leading to misdiagnosis, yet the conditions are distinct and are being managed as separate diseases.
The characteristics of what is known about each condition is described here, and as well for two co-morbidities, Postural Orthostatic Tachycardia Syndrome and Mast cell Activation Syndrome intimately linked to the physiological dysfunctions of the chronic conditions.
The pathophysiological changes in immunological function, neurological regulation, metabolism and energy production, and the microbiome affecting the gut-immune brain axis are discussed and compared for each condition.
The difficulties encountered for diagnosis, and the current lack of effective treatment option are highlighted.
Evidence is presented that affected patients have pressing needs, and that there are currently barriers that prevent access to more effective health support, result in patients being isolated lifelong from employment, and that block access to the essential social services.
Effective public health policy is needed to ensure these inadequacies in public health support are overcome, and financial support is provided to ensure all patients have an enhanced quality of life.
There may be significant benefit for affected patients if research and collective knowledge of these conditions and comorbidities are shared and more integrated, to promote better understanding for their management, provide a wider range of common treatment options, and stimulate more co-ordinated health policies for the management of patient support.
Multiple sclerosis is far better served than the other conditions and could provide the model for how chronic conditions could be managed better.