Sly Saint
Senior Member (Voting Rights)
Scheibenbogen et al
Abstract
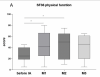
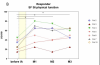
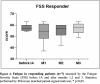
There is increasing evidence for an autoimmune aetiology in post-infectious Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). SARS-CoV-2 has now become the main trigger for ME/CFS. We have already conducted two small proof-of-concept studies of IgG depletion by immunoadsorption (IA) in post-infectious ME/CFS, which showed efficacy in most patients. This observational study aims to evaluate the efficacy of IA in patients with post-COVID-19 ME/CFS. The primary objective is to assess the improvement in functional ability. Due to the urgency of finding therapies for post-Covid-Syndrome (PCS), we report here the interim results of the first ten patients with seven responders defined by an increase of between 10 and 35 points in the Short-Form 36 Physical Function (SF36-PF) at week four after IA. The results of this observational study will provide the basis for patient selection for a randomised controlled trial (RTC) including sham apheresis and for a RTC combining IA with B-cell depletion therapy.
https://www.medrxiv.org/content/10.1101/2023.08.31.23294813v1
Abstract
There is increasing evidence for an autoimmune aetiology in post-infectious Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). SARS-CoV-2 has now become the main trigger for ME/CFS. We have already conducted two small proof-of-concept studies of IgG depletion by immunoadsorption (IA) in post-infectious ME/CFS, which showed efficacy in most patients. This observational study aims to evaluate the efficacy of IA in patients with post-COVID-19 ME/CFS. The primary objective is to assess the improvement in functional ability. Due to the urgency of finding therapies for post-Covid-Syndrome (PCS), we report here the interim results of the first ten patients with seven responders defined by an increase of between 10 and 35 points in the Short-Form 36 Physical Function (SF36-PF) at week four after IA. The results of this observational study will provide the basis for patient selection for a randomised controlled trial (RTC) including sham apheresis and for a RTC combining IA with B-cell depletion therapy.
https://www.medrxiv.org/content/10.1101/2023.08.31.23294813v1