Tom Kindlon
Senior Member (Voting Rights)
Free fulltext:
https://ccs.neu.edu/~ysun/publicati...ity-using-wearable-sensor-and-survey-data.pdf
SYSTEM AND METHODS TO DETERMINE ME/CFS & LONG COVID DISEASE SEVERITY USING WEARABLE SENSOR & SURVEY DATA
by Yifei Sun
A Senior Thesis Submitted to the Faculty of The University of Utah In Partial Fulfillment of the Requirements for the Degree in Bachelor of Science in Computer Science
Abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating disease with high probability of misdiagnosis and significant unmet medical needs that affects as many as 2.5 million people in the U.S. and causes enormous burden for patients, their caregivers, the healthcare system and society. Between 84 to 91 percent of ME/CFS patients are not yet diagnosed [6, 19], and at least one-quarter of ME/CFS patients are house- or bedbound at some point in their lives [12, 13]. The impact of ME/CFS to the U.S. economy, is about $17 to $24 billion in medical bills and lost income from lost household and labor force productivity per year [7, 13].
Current widely used diagnosis methods of ME/CFS and other diseases with similar clinical symptoms like Long COVID [6, 21] are highly dependent on patients’ self reporting [4, 5] and standardized survey, which are not optimal for medical diagnosis. In a joint study with The Bateman Horne Center (BHC) 1 , we designed and developed a system prototype that was able to stably collect terabytes of inertial measurement unit (IMU) time-series data, and analyzed multiple candidate parameters derived from them that could be used as reliable biomarkers for ME/CFS and other diseases with similar clinical symptoms.
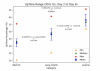
Utilizing our system prototype, MetaProcessor, we conducted grouped t-tests on data collected from the EndoPAT study group (55 recruited, 51 participated, 30 ME/CFS, 15 Long COVID, 6 healthy control) to evaluate the predictive power of Upright Position Time (UpTime), Hours of Upright Activity (HUA), and Steps/Day. Through statistical analysis, we were able to assert the following for ME/CFS versus healthy control: 1. UpTime yielded a low p-value of 0.00004, indicating a significant difference between the groups and demonstrating its potential as a reliable measure for differentiating ME/CFS from healthy control populations. 2. HUA had a p-value of less than 0.00004, suggesting it could also serve as a useful measure for distinguishing ME/CFS from healthy control groups. 3. Steps/Day, x-axis and y-axis, had p-values of 0.01059 and 0.08665, respectively, indicating that step count may be relevant for differentiating ME/CFS individuals from healthy controls, but step count alone may not be sufficient to reliably distinguish between these groups. In a linear regression analysis, we found a moderately positive correlation between UpTime and HUA with r 2 = 0.68. Overall, we can confidently conclude that UpTime is a superior overall predictor due to its objective nature and the lowest p-values observed across all groups.
https://ccs.neu.edu/~ysun/publicati...ity-using-wearable-sensor-and-survey-data.pdf
SYSTEM AND METHODS TO DETERMINE ME/CFS & LONG COVID DISEASE SEVERITY USING WEARABLE SENSOR & SURVEY DATA
by Yifei Sun
A Senior Thesis Submitted to the Faculty of The University of Utah In Partial Fulfillment of the Requirements for the Degree in Bachelor of Science in Computer Science
Abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating disease with high probability of misdiagnosis and significant unmet medical needs that affects as many as 2.5 million people in the U.S. and causes enormous burden for patients, their caregivers, the healthcare system and society. Between 84 to 91 percent of ME/CFS patients are not yet diagnosed [6, 19], and at least one-quarter of ME/CFS patients are house- or bedbound at some point in their lives [12, 13]. The impact of ME/CFS to the U.S. economy, is about $17 to $24 billion in medical bills and lost income from lost household and labor force productivity per year [7, 13].
Current widely used diagnosis methods of ME/CFS and other diseases with similar clinical symptoms like Long COVID [6, 21] are highly dependent on patients’ self reporting [4, 5] and standardized survey, which are not optimal for medical diagnosis. In a joint study with The Bateman Horne Center (BHC) 1 , we designed and developed a system prototype that was able to stably collect terabytes of inertial measurement unit (IMU) time-series data, and analyzed multiple candidate parameters derived from them that could be used as reliable biomarkers for ME/CFS and other diseases with similar clinical symptoms.
Utilizing our system prototype, MetaProcessor, we conducted grouped t-tests on data collected from the EndoPAT study group (55 recruited, 51 participated, 30 ME/CFS, 15 Long COVID, 6 healthy control) to evaluate the predictive power of Upright Position Time (UpTime), Hours of Upright Activity (HUA), and Steps/Day. Through statistical analysis, we were able to assert the following for ME/CFS versus healthy control: 1. UpTime yielded a low p-value of 0.00004, indicating a significant difference between the groups and demonstrating its potential as a reliable measure for differentiating ME/CFS from healthy control populations. 2. HUA had a p-value of less than 0.00004, suggesting it could also serve as a useful measure for distinguishing ME/CFS from healthy control groups. 3. Steps/Day, x-axis and y-axis, had p-values of 0.01059 and 0.08665, respectively, indicating that step count may be relevant for differentiating ME/CFS individuals from healthy controls, but step count alone may not be sufficient to reliably distinguish between these groups. In a linear regression analysis, we found a moderately positive correlation between UpTime and HUA with r 2 = 0.68. Overall, we can confidently conclude that UpTime is a superior overall predictor due to its objective nature and the lowest p-values observed across all groups.