Trajectories of persisting Covid- 19 symptoms up to 24 months after acute infection: findings from the Predi-Covid cohort study
Fischer, Aurélie; Zhang, Lu; Elbéji, Abir; Wilmes, Paul; Snoeck, Chantal J.; Larché, Jérôme; Oustric, Pauline; Ollert, Markus; Fagherazzi, Guy
Long COVID is a multisystemic, fluctuating condition inducing a high burden on affected people. Despite the existence of some guidelines, its management remains complicated. We aimed to demonstrate that symptoms after a COVID-19 infection evolve following different trajectories from the initial infection until 24 months after, to identify the determinants of these trajectories, and the quality of life of people in these trajectories.
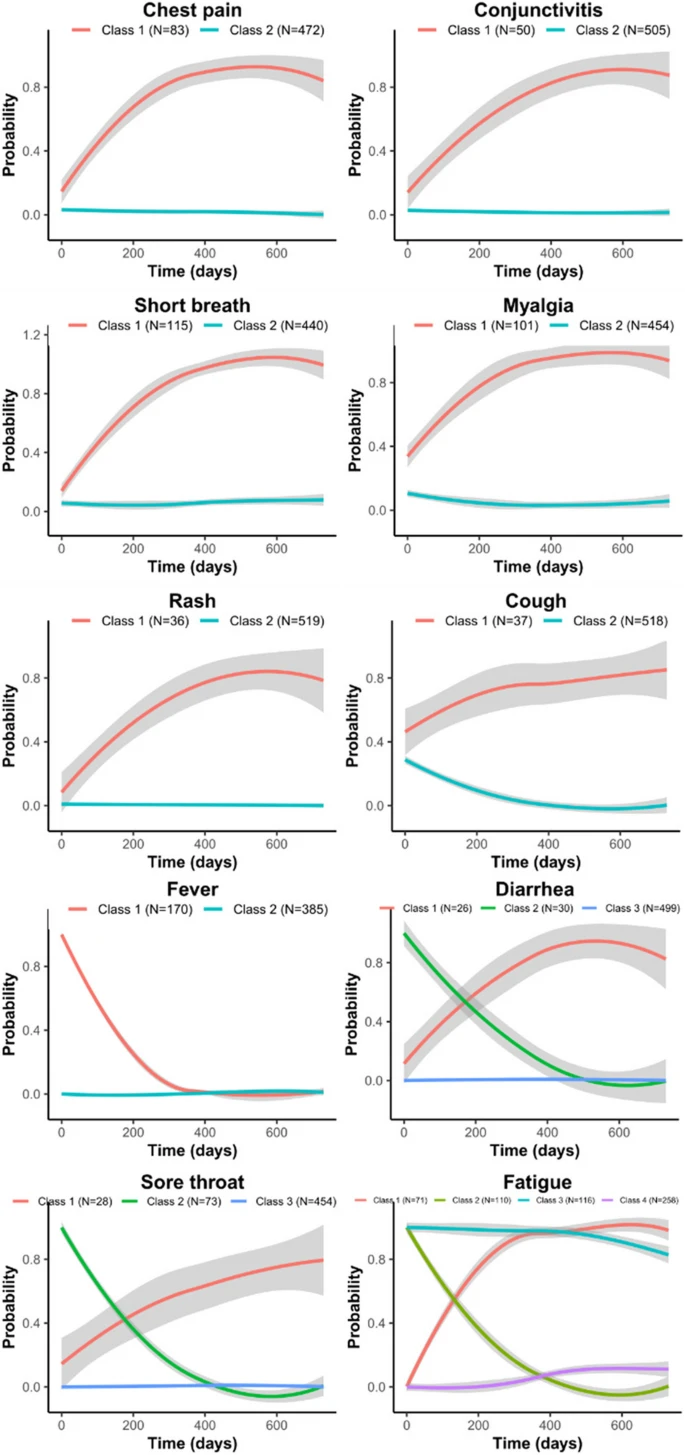
Study participants from the Predi-COVID cohort were digitally followed from their acute SARS-CoV-2 infection until a maximum of 24 months. Data from 10 common symptoms collected at study inclusion, and months 12, 15, and 24 awere used to create a total symptom score. Impact of symptoms on quality of life was assessed at month 24 using standardized questionnaires and ad-hoc questions. Latent classes mixed models were used to identify total score symptom trajectories and individual symptoms trajectories.
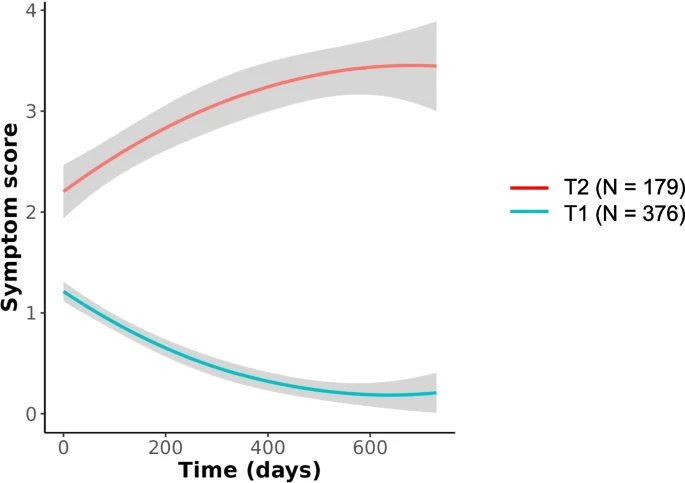
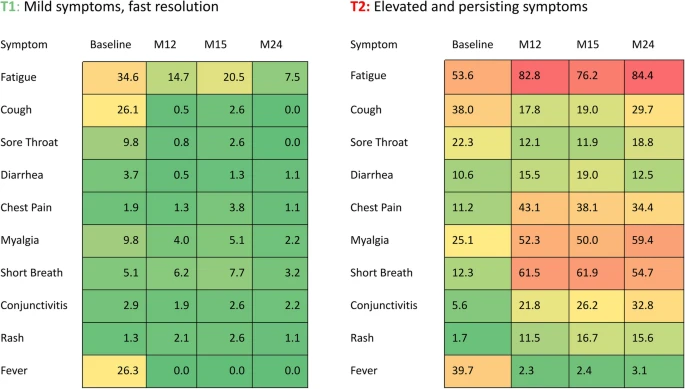
We included 555 participants with at least 2 different time points available during follow-up (Baseline and at least one of the M12, M15 or M24 questionnaires). We identified 2 total symptom score trajectories: T1 “Mild symptoms, fast resolution” (N = 376; 67.7%), and T2 “Elevated and persisting symptoms” (N = 179; 32.3%).
The main determinants of being in T2 were: older age (OR = 1.86; p = 0.003), to be a woman (OR = 1.81; p = 0.001)), elevated BMI (OR = 3.97; p < 0.001), and the presence of multi comorbidities (OR = 2.67; p = 0.005). Symptoms impacted the quality of life more in T2 than in T1 at 24 months (high fatigue level: 64.8% vs 19.5%, altered respiratory quality of life: 42.6% vs 4.6%, anxiety: 24.1% vs 4.6%, stress: 57.4% vs 35.6%, and bad sleep: 75.9% vs 51.1%).
A third of our study population was in the T2 “Elevated and persisting symptoms” trajectory, presenting high symptom frequencies up to 24 months after initial infection, with a significant impact on quality of life. This work underlined the urgent need to better identify individuals most vulnerable to long-term complications to develop tailored interventions for them.
Clinicaltrials.gov NCT04380987 (date of registration: 2020–05-07).
Link | PDF (BMC Infectious Diseases) [Open Access]
Fischer, Aurélie; Zhang, Lu; Elbéji, Abir; Wilmes, Paul; Snoeck, Chantal J.; Larché, Jérôme; Oustric, Pauline; Ollert, Markus; Fagherazzi, Guy
Long COVID is a multisystemic, fluctuating condition inducing a high burden on affected people. Despite the existence of some guidelines, its management remains complicated. We aimed to demonstrate that symptoms after a COVID-19 infection evolve following different trajectories from the initial infection until 24 months after, to identify the determinants of these trajectories, and the quality of life of people in these trajectories.
Study participants from the Predi-COVID cohort were digitally followed from their acute SARS-CoV-2 infection until a maximum of 24 months. Data from 10 common symptoms collected at study inclusion, and months 12, 15, and 24 awere used to create a total symptom score. Impact of symptoms on quality of life was assessed at month 24 using standardized questionnaires and ad-hoc questions. Latent classes mixed models were used to identify total score symptom trajectories and individual symptoms trajectories.
We included 555 participants with at least 2 different time points available during follow-up (Baseline and at least one of the M12, M15 or M24 questionnaires). We identified 2 total symptom score trajectories: T1 “Mild symptoms, fast resolution” (N = 376; 67.7%), and T2 “Elevated and persisting symptoms” (N = 179; 32.3%).
The main determinants of being in T2 were: older age (OR = 1.86; p = 0.003), to be a woman (OR = 1.81; p = 0.001)), elevated BMI (OR = 3.97; p < 0.001), and the presence of multi comorbidities (OR = 2.67; p = 0.005). Symptoms impacted the quality of life more in T2 than in T1 at 24 months (high fatigue level: 64.8% vs 19.5%, altered respiratory quality of life: 42.6% vs 4.6%, anxiety: 24.1% vs 4.6%, stress: 57.4% vs 35.6%, and bad sleep: 75.9% vs 51.1%).
A third of our study population was in the T2 “Elevated and persisting symptoms” trajectory, presenting high symptom frequencies up to 24 months after initial infection, with a significant impact on quality of life. This work underlined the urgent need to better identify individuals most vulnerable to long-term complications to develop tailored interventions for them.
Clinicaltrials.gov NCT04380987 (date of registration: 2020–05-07).
Link | PDF (BMC Infectious Diseases) [Open Access]
Last edited: