Dakota15
Senior Member (Voting Rights)
Post copied from US News, and some subsequent posts moved
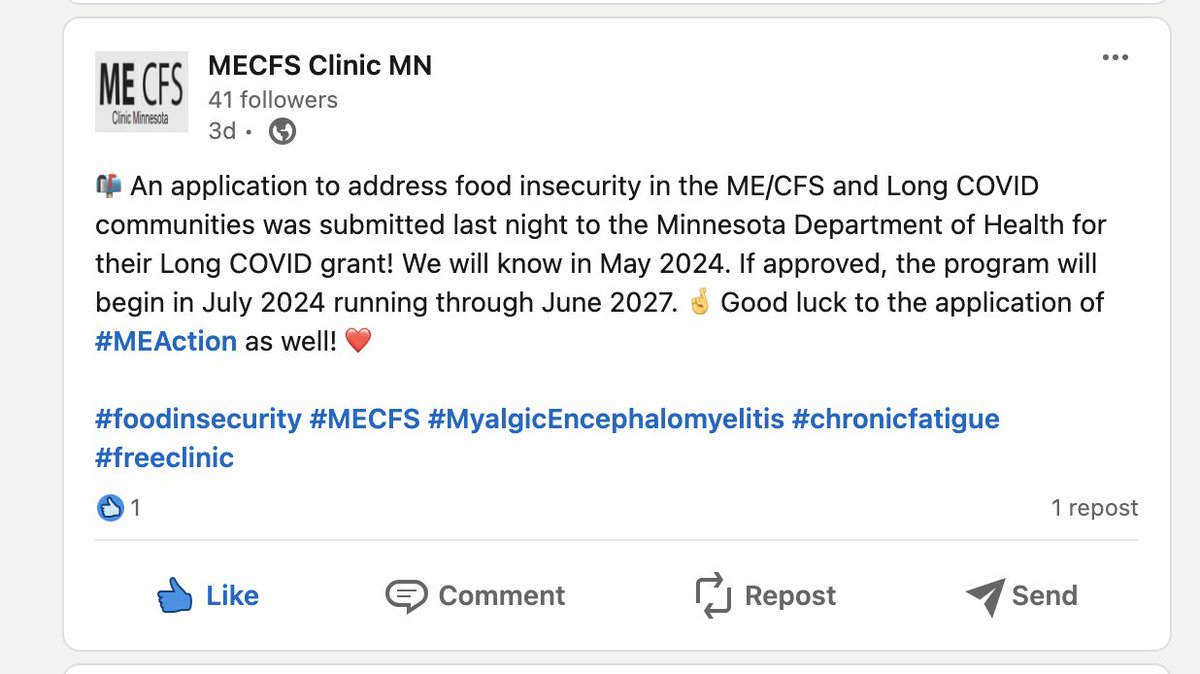
Sharing one of the lead stories on our evening news tonight in Minneapolis, MN. This is the third ME / LC feature this reporter and station has spotlighted since December. Some of you may also be familiar with Dr. Ruby Tam or ME/CFS Clinic Minnesota.
KSTP News (ABC Affiliate): 'Minnesota’s first ME/CFS doctor on a mission to expand care to ‘everybody who has the disease’’
''It’s a debilitating disease associated with profound exhaustion, and it’s recently become intertwined with long COVID.'
‘...I owe everybody who has the disease a responsibility to get the care they need to them, either myself or educate their local providers and practitioners to help get them better.”
Sharing one of the lead stories on our evening news tonight in Minneapolis, MN. This is the third ME / LC feature this reporter and station has spotlighted since December. Some of you may also be familiar with Dr. Ruby Tam or ME/CFS Clinic Minnesota.
KSTP News (ABC Affiliate): 'Minnesota’s first ME/CFS doctor on a mission to expand care to ‘everybody who has the disease’’
''It’s a debilitating disease associated with profound exhaustion, and it’s recently become intertwined with long COVID.'
‘...I owe everybody who has the disease a responsibility to get the care they need to them, either myself or educate their local providers and practitioners to help get them better.”
Last edited by a moderator: