I'm wondering this in the context of the kind of unpleasant life-long drugs we might end up on if @Jonathan Edwards's
paper on Qeios is right about what's wrong with us, and if we would fall into the category of 'diseases that can never be cured'.
I don't think I said anything about life long nasty treatments or not curing ME/CFS. If our proposal on Qeios is right then re-balancing T cell populations ought to return the system to normal. If the rogue T cells are an overexpanded CD4 cyttoxic population then a single dose of the right monoclonal antibody might sort that in a couple of hours. But clearly things are complicated, with various possibilities, some of which might require longer term treatment until we have the right technology.
The answer to the question about why some diseases are curable is a full term's worth of pathology lectures. But there are some simple bits.
Many diseases are defined by the presence of cells with a new packet of disease instructions written in DNA. So every morning you wake up with all the healthy instructions you were born with plus these bad instructions. If you have the disease haemophilia you were born with bad instructions in all cells, including the ones that are supposed to make blood clotting factors. Curing purely genetic disease is now becoming possible by adding in the missing instructions by gene therapy.
In infectious disease the DNA instructions are in the bacteria or viruses. Curing simply requires getting rid of the microbes with their instructions. If it is a virus that incorporates its instructions into your cells it is potentially trickier but most of those infections are not widespread. In AIDS the instructions are mostly only incorporated into lymphocytes I think and you can make new ones.
Some diseases occur because time and environment acting on a body built with good instructions end up making it deteriorate. Smoking destroys lung airspaces. Some people are born with genes that code for joints falling apart sixty years later - osteoarthritis. You can cure that with a hip replacement in a sense. But very often the instructions for building a body cannot be used to repair it. It is a bit like a potter who, after lengthy work at the wheel finds the pot has developed an asymmetry. There is nothing she can do on the wheel to put this right. It always progresses until the pot fails. The growth of a joint with two surfaces that fit exactly right cannot be re-run using the DNA that made it. You would have to grow a new entire joint in a petri dish and transplant it.
High blood pressure is another disease where it seems that under certain influences the vessel structures that have been built progressively get less and less good at regulating pressure up or down and once pressures start to rise they tend to go on rising. Hard to cure without re-building the vessels from scratch.
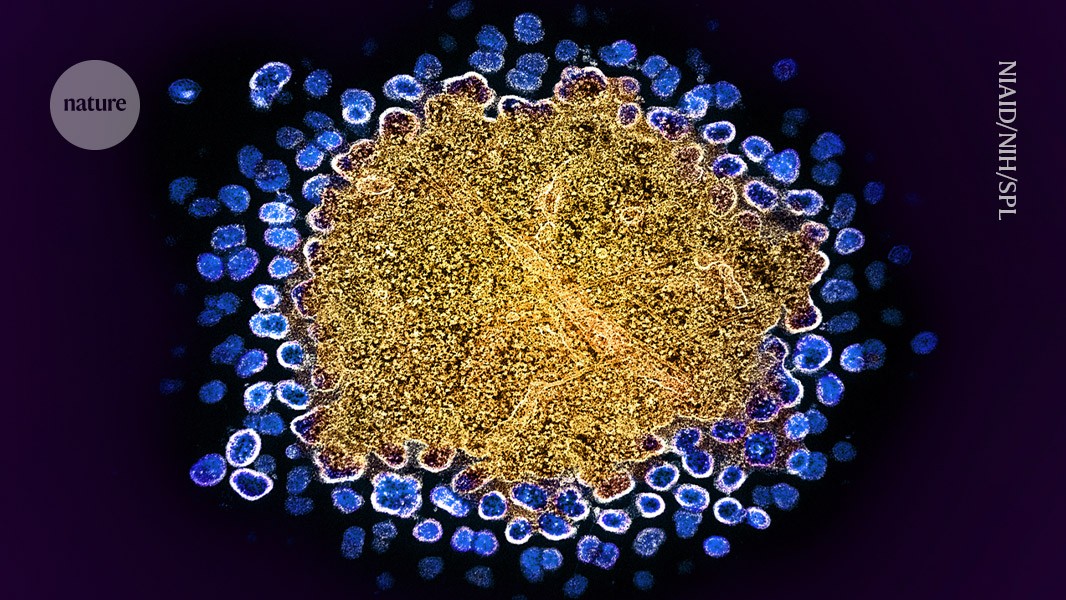
For diseases of the immune system like RA and lupus, and I am now prepared to bet ME/CFS, the problem mostly seems to be that over time you generate lymphocytes that vary in their instructions deliberately (to deal with different infections) and there are certain ways that, again, a shift in the stock of the library of instructions tends to perpetuate itself. The cells with dodgy instructions tell each other to make more copies of themselves. There are examples where the problem can right itself or be abolished as in the case of immune thrombocytopenia cured by rituximab. But in most cases it is hard to clear out enough of the cells with the wrong instructions. I think we coud have done that by now if people put their minds to it and it will be done in the future but it has been very slow progress since 2000.
Cancer of course is due to all the offspring of a single cell that developed a mistake in its DNA instructions that led to more mistakes and a failure of control of division as a result. Curing depends on getting rid of every one of the cells or at last so many that the last few get cleared away by the immune system. You can of course of cut the cells out in one go. Lots of cancers are now curable. Ironically, cancer is the most curable of all diseases. That has been achieved by really focused research. The same should have been done for RA and lupus and the same should be done for ME/CFS. Everything I see [points to it being a reversible problem. Genetic risk factors will still be there but they do not in themselves make the disease.