Andy
Senior Member (Voting rights)
Full title: A multivariate Swedish national twin-sibling study in women of major depression, anxiety disorder, fibromyalgia, and irritable bowel syndrome
Abstract
Background
Functional Somatic Disorders (FSD) and Internalizing Psychiatric Disorders (IPD) are frequently comorbid and likely share familial/genetic risk factors.
Methods
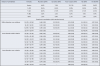
We performed a Common Factor Multivariate Analysis of 2 FSDs, Fibromyalgia (FM) and Irritable Bowel Syndrome (IBS), and two IPDs, Major Depression (MD) and Anxiety Disorders (AD), in five kinds of Swedish female–female relative pairs: monozygotic (n = 8,052) dizygotic (n = 7216), full siblings (n = 712,762), half-siblings reared together (n = 23,623), and half-siblings reared apart (n = 53,873). Model fitting was by full information maximum likelihood using OpenMx.
Results
The best-fit model included genetic, shared environmental, and unique environmental factors. The common factor, ~50% heritable with a small shared environmental effect, loaded more strongly on the two IPDs (~0.80) than the 2 FSDs (0.40). Disorder-specific genetic effects were larger for the 2 FSDs (~0.30) than the 2 IPDs (~0.03). Estimated genetic correlations were high for MD and AD (+0.91), moderate between IBS and IPDs (+0.62), and intermediate between FM and MD (+0.54), FM and AD (+0.28), and FM and IBS (+0.38). Shared environmental influences on all disorders were present but small.
Conclusions
In women, FSDs and IPDs shared a moderate proportion of their genetic risk factors, greater for IBS than for FM. However, the genetic sharing between IBS and FM was less than between MD and AD, suggesting that FSDs do not form a highly genetically coherent group of disorders. The shared environment made a modest contribution to the familial aggregation of FSDs and IPDs.
Open access
Abstract
Background
Functional Somatic Disorders (FSD) and Internalizing Psychiatric Disorders (IPD) are frequently comorbid and likely share familial/genetic risk factors.
Methods
We performed a Common Factor Multivariate Analysis of 2 FSDs, Fibromyalgia (FM) and Irritable Bowel Syndrome (IBS), and two IPDs, Major Depression (MD) and Anxiety Disorders (AD), in five kinds of Swedish female–female relative pairs: monozygotic (n = 8,052) dizygotic (n = 7216), full siblings (n = 712,762), half-siblings reared together (n = 23,623), and half-siblings reared apart (n = 53,873). Model fitting was by full information maximum likelihood using OpenMx.
Results
The best-fit model included genetic, shared environmental, and unique environmental factors. The common factor, ~50% heritable with a small shared environmental effect, loaded more strongly on the two IPDs (~0.80) than the 2 FSDs (0.40). Disorder-specific genetic effects were larger for the 2 FSDs (~0.30) than the 2 IPDs (~0.03). Estimated genetic correlations were high for MD and AD (+0.91), moderate between IBS and IPDs (+0.62), and intermediate between FM and MD (+0.54), FM and AD (+0.28), and FM and IBS (+0.38). Shared environmental influences on all disorders were present but small.
Conclusions
In women, FSDs and IPDs shared a moderate proportion of their genetic risk factors, greater for IBS than for FM. However, the genetic sharing between IBS and FM was less than between MD and AD, suggesting that FSDs do not form a highly genetically coherent group of disorders. The shared environment made a modest contribution to the familial aggregation of FSDs and IPDs.
Open access