Codeveloping a Novel Intervention for People With Post-COVID Condition: The Balance-ACT Study
Lily Felton; Michail Kalfas; Debbie Brewin; Carole Beckwith; Tasbiha Khan; Caroline Jolley; Nicholas Hart; Emma L. Duncan; Timothy Nicholson; Oliver Witard; Julie Moore; Alan Metcalfe; Gerrard F Rafferty; Trudie Chalder
INTRODUCTION
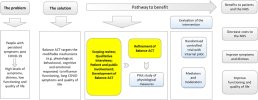
Some people experience persistent symptoms, such as fatigue, brain fog and breathlessness, long after the onset of COVID-19 infection. This is known as the post-COVID syndrome (PCS). We developed a unique and holistic psycho-physiological intervention that integrates Acceptance and Commitment Therapy (ACT), a structured talking therapy, with principles of homeostasis. This aims to provide targeted support and treatment strategies for effectively managing the long-term repercussions of the condition and improve patient outcomes.
METHODS
This empirical study was informed by theory and other research strands. These strands included a qualitative study of people with lived experience, a scoping review of interventions for fatigue (including rehabilitation) and insights from a patient and public involvement (PPI) group. The PPI group were actively involved in the development of the intervention, manuals and overall study management, ensuring it was relevant, ethical and aligned with patient preferences and needs.
RESULTS
The qualitative study uncovered the tangible contexts in which the intervention would be implemented, and the attraction of Balance-ACT for those living with PCS. People living with PCS (n = 19) and health care professionals (HCPs; n = 12) provided overall endorsement for the intervention. Through an iterative process, their feedback, alongside input from the PPI group, informed the development of key materials, including a therapist manual, participant handbook, mindfulness recordings and an animation. Therapists were trained, and a novel fidelity measure was developed to ensure adherence to Balance-ACT principles.
CONCLUSION
We used an iterative approach to develop the Balance-ACT intervention, which was acceptable to patients and HCPs. Subsequent research will examine the efficacy of Balance-ACT.
PATIENT AND PUBLIC CONTRIBUTION
This article represents work conducted as part of the Balance-ACT project. People with the post-COVID condition (PCC) were involved throughout all aspects of this study, in line with the National Institute for Health and Care Research framework, and contributed in several key ways. It ensured the research captured a diverse range of illness experiences. The study design was refined and addressed potential barriers to engagement. Patient-friendly language was used to improve accessibility, making the study more inclusive. Additionally, the outcome measures were informed by patient input to enhance their relevance. Finally, dissemination was guided to ensure that the findings were both useful and accessible, using clear language in reporting and incorporating feedback from patient representatives on drafts to ensure clarity.
Link | PDF (Health Expectations) [Open Access]
Lily Felton; Michail Kalfas; Debbie Brewin; Carole Beckwith; Tasbiha Khan; Caroline Jolley; Nicholas Hart; Emma L. Duncan; Timothy Nicholson; Oliver Witard; Julie Moore; Alan Metcalfe; Gerrard F Rafferty; Trudie Chalder
INTRODUCTION
Some people experience persistent symptoms, such as fatigue, brain fog and breathlessness, long after the onset of COVID-19 infection. This is known as the post-COVID syndrome (PCS). We developed a unique and holistic psycho-physiological intervention that integrates Acceptance and Commitment Therapy (ACT), a structured talking therapy, with principles of homeostasis. This aims to provide targeted support and treatment strategies for effectively managing the long-term repercussions of the condition and improve patient outcomes.
METHODS
This empirical study was informed by theory and other research strands. These strands included a qualitative study of people with lived experience, a scoping review of interventions for fatigue (including rehabilitation) and insights from a patient and public involvement (PPI) group. The PPI group were actively involved in the development of the intervention, manuals and overall study management, ensuring it was relevant, ethical and aligned with patient preferences and needs.
RESULTS
The qualitative study uncovered the tangible contexts in which the intervention would be implemented, and the attraction of Balance-ACT for those living with PCS. People living with PCS (n = 19) and health care professionals (HCPs; n = 12) provided overall endorsement for the intervention. Through an iterative process, their feedback, alongside input from the PPI group, informed the development of key materials, including a therapist manual, participant handbook, mindfulness recordings and an animation. Therapists were trained, and a novel fidelity measure was developed to ensure adherence to Balance-ACT principles.
CONCLUSION
We used an iterative approach to develop the Balance-ACT intervention, which was acceptable to patients and HCPs. Subsequent research will examine the efficacy of Balance-ACT.
PATIENT AND PUBLIC CONTRIBUTION
This article represents work conducted as part of the Balance-ACT project. People with the post-COVID condition (PCC) were involved throughout all aspects of this study, in line with the National Institute for Health and Care Research framework, and contributed in several key ways. It ensured the research captured a diverse range of illness experiences. The study design was refined and addressed potential barriers to engagement. Patient-friendly language was used to improve accessibility, making the study more inclusive. Additionally, the outcome measures were informed by patient input to enhance their relevance. Finally, dissemination was guided to ensure that the findings were both useful and accessible, using clear language in reporting and incorporating feedback from patient representatives on drafts to ensure clarity.
Link | PDF (Health Expectations) [Open Access]