Merged thread
New Lancet publication from Trudie Chalder and crew.
This is perhaps rather long but I think important background information for the ME world.
Not specific to ME; however, as dissociative seizures are poorly understood and have been psychologised a great deal, it is interesting to compare how poorly the model of CBT fared here. Sometimes IAPT have tried to include DS under MUS. The last list of IAPT MUS's I saw it had dropped off the list. Probably because someone objected loudly

Here is the paper:
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(20)30128-0/fulltext?fbclid=IwAR1eZLXCsM61_bzgxwpqXlNf81QvoUKS6H0ISdPIJnhSsD-iLWh2KPyOZxQ
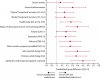
CBT did not reduce the patient recorded and reported number of seizures - the primary outcome. The trial very modestly improved a few psychosocial measures - but that could be placebo given the nature of the study - clinician's can't be blinded to what they are doing - neither are the patients.
What stands out for me was how ineffective it was at reducing the initial modest levels of distress these patients have. Plus, the very high level of physical disability - which were also unaffected by the intervention. No mention about that in the paper. The researchers seem blind to this.
I've worked with many patients with epilepsy via my clinic at The Brain Charity in Liverpool and DS came up fairly frequently. Many patients with diagnosed epilepsy also have some DS's. Patients tend to see them as physical. They and 'do and don't' buy into the psychological explanation - it causes cognitive dissonance and they tend to put this aside and try and cope. It's quite marmite. I have helped people to mange and cope with them. People were generally quite stable medically when I'd see them so this is perhaps a different patients cohort to those seen in neurology clinics earlier on in the process. If there was PTSD/trauma reaction then I'd happy work on that with the patient, if they felt it was relevant, but I'd not suspect that this would reduce seizures or frequent - that might be nice if it happened (as in less stress as a trigger) but I'd not 'sell' it that way.
The CBT of model of DS is
“Adapted specifically for patients with DS, the intervention was based on models of fear-avoidance 4,5”
Isn’t everything is TC et al’s world ‘fear avoidance’. We have seen this before!
And here are those references - check out the dates:
4 Lang PJ. Fear reduction and fear behaviour: problems in treating a construct. In: Shilen JM, ed. Research in Psychotherapy (Vol III). Washington DC: American Psychological Association;
1968.
5 Mowrer OH. Learning theory and behaviour. New York: Wiley;
1960.
From the main paper – on average the levels of anxiety and low mood (GAD7 & PHQ9) (Table 2) are modest and pretty low overall and remain unchanged over the intervention. Does not suggest this is a distress / psychologically driven condition. pwPTSD or depression score near the maximum on these two forms - pretty much universally. If I was referred modest/low distressed patients with trauma I'd suspect they were functioning emotionally pretty well..... so I'd be querying the diagnosis.
More from Table 2 - These patients are physically really debilitated (SF-12 score around 40 pre and post – out of max score of 100). My PTSD patients (non-injurious ones) are not physically disabled at all. My panic/agoraphobia patients are well physically usually. What’s with the v low physical functioning? That’s completely missed.
From the supplementary information: CBT for DS is supposed to be similar to that for CBT for panic / trauma along with assuming the patients are dissociating during an attack – i.e. a coping mechanism along with avoidance re previous trauma. OK, well I treat all of that using trauma focused CBT and I get a high recovery rate and there is a good evidence base for this. My patients will start of scoring high/max on PHQ9 / GAD7 and end up low/close to zero by the end. So, why doesn’t CBT work in DS? Suggests strongly to me that the model is wrong. There is no voice in this work for the patients experience of the therapy. That could be illuminating.
Also, having read what is covered in therapy (pages 7 and 8 of the supplementary info) it is NOT close to CBT for panic or trauma at all. There is no psychoeducation re fight, flight, freeze response (FFF) and adrenaline/cortisol reaction etc and normalisation of this response – a big part of CBT for panic. Along with the importance of examining and reframing the cognitive processes of the impeding catastrophe that is usually predicted by panic patients in response to benign bodily symptoms of the FFF response- i.e. "I'm going to die / have a heart attack / faint / cause a scene" and so forth.
Here we have something else: Relaxation, breathing techniques and distraction is used/taught in CBT for DS – but these are by definition cognitive and behavioural avoidance strategies…… Duh – you could not make it up if you tried.
The CBT potentially taught them how to be more avoidant! There was little exploration of previous traumas. When it is there, there is no structured approach to working on the narrative / meaning and the updating of trauma narrative / meaning so that they can move on from their trauma (if relevant – it is assumed to be relevant though – psychometrics don’t suggest severe impact of trauma). In summary, during CBT – patients experience training in how to carry on avoiding upsetting feelings and thinking. Words fail me.
75% compliance is pretty low – i.e. attended 9 out of 12 sessions or more. I'd expect 90% or more for such a brief intervention if patients were engaged - and that's not the patients fault - it suggests there was a significant group that did not buy into this.
From the supplementary material:
“CBT specifically focuses on reducing DS and arousal and emotional/behavioural avoidance, enabling people to reengage in activities of everyday life.” How did they assess this post intervention? I can’t see how they did this. In PTSD the PTSD cognitions questionnaire can be a helpful measure. A shift in thinking about how people respond to trauma symptoms goes hand in hand with reduced distress and patient recovery. How come nothing like that was used here to evaluate if the patients actually are less avoidant post CBT? Partly because I fear that their CBT intervention taught them to be more behaviourally and cognitively avoidant – good grief.
Psychiatric assessment at 3 months - process – structured? No mention of using the SCID. Reads more like a bit of a chat rather than robust process. It needed to be robust. Otherwise this is meaningless.
Use of self complete Mini-International Neuropsychiatric Interview (MINI) (no match for a clinician administered SCID) and Standardised Assessment of Personality-abbreviated Scale (SAPAS-SR) for maladaptive personality traits. Pretty much anyone who was irritable, annoyed, upset, distressed or traumatised after developing poorly understood debilitating condition will score 'positive' on this rubbish scale (e.g. > 3):
You’ll get my drift when you read the 8 Q’s:
https://www.nhshighland.scot.nhs.uk/Services/Documents/Personality disorder service/3 Assessment/SAPAS.pdf
This is a questionnaire that at best should lead into a discussion as to how relevant a positive response is – and being impulsive, irritable, a bit of a worrier, need to depend on others, and so forth could all be raised when developing a distressing medical condition…….. that needs separating out otherwise it’s going to provide a high number of false positives/misleading data. But it helps to bolster the view that DS are a problem caused by patients dodgy coping / personality. Lovely.
“58% had SAPAS-SR scores suggestive of maladaptive personality traits” – now that’s pretty leading – if this is turned around it can be said that 42% of the patients had no hint of personality issues – that’s a big chunk of people. Personality disorders are notoriously controversial and are often a consequence of trauma – so complex PTSD would perhaps be a more useful ‘label’ (if one is needed) for the majority of the time – context is all here. And they used a self-report form of this questionnaire (see above) so there is massive scope for misunderstanding / misinterpretation of what is being assessed / asked about and for positive result where no ‘problems’ exist. Personality disorder is usually a lazy psychiatric diagnosis which does not tell much about how a person ended up where they have done (personality wise). i.e. it is not in context or that meaningful for the patient – stigmatising (minimises the impact of trauma and social context and places the ‘disorder’ within the person) rather than being helpful. Again this was not well assessed (and this needs to be). Raised scores on the SAPAS-SR could easily be a consequence of developing distressing condition. Or in part due to deprivation. Or lots of things like autism or brain injury or just being a human. Not to mention the upset as a result of breaches of trust in medical circumstances.
Use of multiple self competed forms - GAD, PHQ, WSAS, Visual analogue scales, CORE, PHQ-15, Global impression of improvement, SF-12, etc. All these subjective measures are open to bias.
DS diagnosis versus epilepsy:
Video EEG? Limitations of EEG? My understanding is that EEG measures electrical activity over the scalp. This is then interpreted as being a measure of brain activity. However, I can’t see how this this assesses deep brain activity away from the surface? My question for my neurology colleagues is: Is it not possible DS are deeper brain disruption as opposed to whole brain disruption in epilepsy? Is that even possible? Frontal lobe epilepsy is often missed by EEG..... I wonder if anyone can comment here?
Me thinks that overall: DS patients have not been well assessed or understood and largely psychiatrised / psychologised. More work is, I think, needed here to actually understand the phenomenon. For example, frontal lobe epilepsy is often missed by EEG…... So, in summery – epilepsy remains a clinical diagnosis – so uncertainty is everywhere. And when that’s present in spades – it therefore must be the patient that is the ‘problem’. It’s a bit weak this tired argument and I suspect lacks much face validity.
From Mellers (2004) (one of the co-authors of the CBT trial) (
https://pmj.bmj.com/content/postgradmedj/81/958/498.full.pdf):
“According to Chadwick50 the EEG is “one of the most abused investigations in clinical medicine and is unquestionably responsible for great human suffering”. While a single routine EEG may be normal in some 30% of patients with epilepsy (the false negative rate falls to around 15%, or even less in patients with repeated studies or sleep recordings51) Chadwick was highlighting the problem of false positives. Anything up to 15% of the normal population may have a “non-specific” abnormality noted on EEG. There is clearly a danger both that an EEG may be “over reported”, especially if the request form sent to the electrophysiologist expresses no doubt about the diagnosis, and also that such non-specific abnormalities might be misunderstood by inexperienced clinicians as backing a diagnosis of epilepsy when they do no such thing. This problem is compounded by the fact that such non-specific abnormalities (principally a slow background rhythm) are more common in patients with DS than in healthy volunteers52 and in patients with borderline personality disorder,53 which is common in patients with DS (see below). It should be noted, however, that rigorously defined specific “epileptiform” abnormalities (generalised spikes or polyspike and slow wave abnormalities) are very rare (about 3 in 1000) in healthy people.54,55 The EEG is just one factor that must be weighed up in making a diagnosis of epilepsy that ultimately rests on clinical judgement.” So in summary – plenty room for misdiagnosis / misunderstanding…. Sounding familiar?
So in summary:
- The outcome failed because CBT model they used had no impact on the mechanism causing DS.
- And the intervention failed because it didn’t even target the trauma / panic / dissociation.
This is frustrating and a lost opportunity.
In the commentary by Perez (Harvard):
https://www.thelancet.com/pdfs/journals/lanpsy/PIIS2215-0366(20)30143-7.pdf
"The first question is whether seizure frequency should be the preferred primary outcome measure in clinical trials for dissociative seizures."
So, the research community might move towards smudging the issue and moving towards using more subjective outcome measures – which is not helpful as this will be biased by what you expect the patients to learn / understand during therapy. And as such a trial cannot be blinded to the clinicians undertaking the therapy it ideally needs to involve an objective, primary, real world relevant outcome measure - seizure frequency. That much the CBT research world should have learned from PACE.
His second question re 'one size fits all' is important:
What Perez is saying is that there needs to be subgrouping – and I agree here, for example:
- e.g. DS plus PTSD – identify and treat that (there is a good solid evidence base for trauma therapy) and does that have an effect on DS frequency? That does need to be studied.
- Ditto panic disorder
- Ditto personality disorder (if that is necessary? They probably largely come under PTSD when examined via SCID).
- DS patients with low levels of distress. Now that’s a bit more tricky but necessary as overall these patients are not highly distressed. This will form quite a large group of DS patients.
- DS and the impact of physical therapy – does activity trigger a DS? I wonder if that has ever been studied? Objectively measured would be ideal. I’ve not looked. Their levels of physical disability are really high. Why? What other symptoms do they have? Pain? PEM? It’s absent from the literature but patients talk about it on forums and in responses to online articles.
Studying those might be helpful. If that work is done well with independent assessors pre and post, uses SCID and appropriate psychometrics pre and post interventions using the evidence based model and dose of CBT and so forth it might reveal a lot.
From Perez: "In my opinion, CBT remains an effective treatment for dissociative seizures. I have witnessed how some patients with dissociative seizures can benefit greatly from a CBT approach that equips the patient with new psychotherapeutic tools, which in certain individuals can lead to robust and sustained clinical improvement." Me thinks that is called
eminence based medicine. We can't role out ineffective CBT to everyone without knowing the subgroup of patients this does work in - if at all - based on what a chap at Harvard says so. As a psychologist I suspect his view is impacted by his selective recall of one to two patients who improved a lot - but were they cured? Were they largely PTSD anyway? Were these few patients misdiagnosed? CBT can help with tolls to cope well - but that was not what this trial was about. And it failed in that endeavour too - no real world, significant reduction in distress.
Joan Crawford
Counselling Psychologist
UK