Tom Kindlon
Senior Member (Voting Rights)
Pre-print
Free fulltext:
https://www.researchsquare.com/article/rs-3164397/v1
Comparison of T-cell Receptor Diversity of people with Myalgic Encephalomyelitis versus controls
Joshua J Dibble1
Ben Ferneyhough2
Matthew Roddis2
Sam Millington2
Michael D Fischer2
Nick J Parkinson2
Chris P Ponting1
Email
1 University of Edinburgh,
2 Systems Biology Laboratory UK
Objective:
Myalgic Encephalomyelitis (ME; sometimes referred to as Chronic Fatigue Syndrome or CFS) is a chronic disease without laboratory test, detailed aetiological understanding or effective therapy. Its symptoms are diverse, but it is distinguished from other fatiguing illnesses by the experience of post-exertional malaise, the worsening of symptoms even after minor physical or mental exertion. Its frequent onset after infection might indicate that it is an autoimmune disease or that it arises from abnormal T-cell activation.
Results:
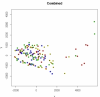
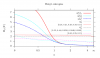
To test this hypothesis, we sequenced the genomic loci of a/d, b and g T-cell receptors (TCR) from 40 human blood samples from each of four groups: severely affected people with ME/CFS; mildly or moderately affected people with ME/CFS; people diagnosed with Multiple Sclerosis, as disease controls; and, healthy controls. Seeking to automatically classify these individuals’ samples by their TCR repertoires, we applied P-SVM, a machine learning method. However, despite working well on a simulated data set, this approach did not partition samples into the four subgroups, beyond what was expected by chance alone. Our findings do not support the hypothesis that blood samples from people with ME/CFS frequently contain altered T-cell receptor diversity.
Free fulltext:
https://www.researchsquare.com/article/rs-3164397/v1
Comparison of T-cell Receptor Diversity of people with Myalgic Encephalomyelitis versus controls
Joshua J Dibble1
Ben Ferneyhough2
Matthew Roddis2
Sam Millington2
Michael D Fischer2
Nick J Parkinson2
Chris P Ponting1
1 University of Edinburgh,
2 Systems Biology Laboratory UK
Objective:
Myalgic Encephalomyelitis (ME; sometimes referred to as Chronic Fatigue Syndrome or CFS) is a chronic disease without laboratory test, detailed aetiological understanding or effective therapy. Its symptoms are diverse, but it is distinguished from other fatiguing illnesses by the experience of post-exertional malaise, the worsening of symptoms even after minor physical or mental exertion. Its frequent onset after infection might indicate that it is an autoimmune disease or that it arises from abnormal T-cell activation.
Results:
To test this hypothesis, we sequenced the genomic loci of a/d, b and g T-cell receptors (TCR) from 40 human blood samples from each of four groups: severely affected people with ME/CFS; mildly or moderately affected people with ME/CFS; people diagnosed with Multiple Sclerosis, as disease controls; and, healthy controls. Seeking to automatically classify these individuals’ samples by their TCR repertoires, we applied P-SVM, a machine learning method. However, despite working well on a simulated data set, this approach did not partition samples into the four subgroups, beyond what was expected by chance alone. Our findings do not support the hypothesis that blood samples from people with ME/CFS frequently contain altered T-cell receptor diversity.