‘Abysmal’ communication blamed for variations in self-isolation list
By
Lawrence Dunhill12 June 2020
A rushed and confused process has resulted in huge variation in the national list of extremely vulnerable people advised to self-isolate from coronavirus,
HSJ has found.
In some areas of the country, particularly parts of Merseyside, clinical commissioning groups have been heavily involved in the process of building the “shielding patient list” – using local databases to carry out comprehensive searches and adding large numbers of patients.
In other areas, there has been little involvement from local commissioners, with the task of validating and adding patients to the list primarily carried out by GPs. These areas appear to have added far fewer patients to the list.
It means people with very similar needs are potentially being treated differently depending on where they live.
At the start of the pandemic, work was started to identify “extremely vulnerable” people – such as cancer patients and organ transplant recipients – who were at high risk of becoming seriously ill from covid-19 and would need to completely self-isolate. They are eligible for food parcels and deliveries of medication.
The process was begun by NHS Digital and NHS England, which identified around 1.3 million people using nationally held lists. Local GPs were then asked on 23 March to validate the national list and add patients where necessary, and to do this within seven days.
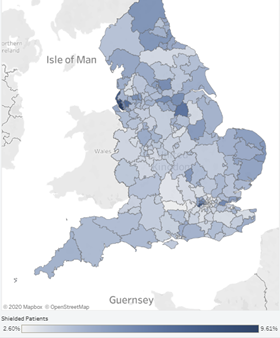
NHS Digital map showing the proportion of shielding patients in each CCG
In some places, such as Liverpool, South Sefton and Southport and Formby, CCGs effectively coordinated the process for their member practices, and reacted quickly to the initial guidance.
Liverpool CCG, for example, led searches of patient records on GPs’ IT systems, with the results then reviewed by GPs. This resulted in Liverpool’s list growing more than four-fold from the initial nationally compiled list, from 11,000 to 48,000. Around 10 per cent of the population is now on the shielding list. A spokeswoman said the CCG was not under any pressure to reduce its list.
South Sefton and Southport and Formby CCGs declined to provide detailed numbers to show how many patients were added locally. But a spokeswoman confirmed their “clinically designed searches” were coordinated by the CCG and local medical committee, on behalf of GP practices. Their lists represent 9 per cent and 8 per cent of the population respectively.
Although a degree of higher need is expected in these areas, other areas which might be expected to have similar needs, such as Manchester and Blackpool have just 4 and 5 per cent of their population on the list.
Manchester’s list increased less than two-fold after the local validation, from 13,000 to 22,000. When asked how its list was compiled, the CCG cited updated guidance that was issued by NHS Digital in late April, which said “no automated searches” should be carried out locally by CCGs.
A spokesman said GPs validated their own lists with CCG involvement limited to providing support and updates on the process, and also suggested the older age profile in Liverpool “probably explains” the difference in relative list size.
But the disparity in the shielding lists when looking solely at the population over 70 is even greater. Around 37 per cent of over 70s in Liverpool’s are on the list – the highest proportion in the country alongside Hounslow in west London - compared to 17 per cent in Manchester.
Blackpool CCG did not provide numbers for patients identified locally, but appears to have followed a similar process to Manchester.
Hounslow, which has 8 per cent of its total population on the list, appears to be an outlier in London. Its list grew more than four-fold, from an initial 3,000 identified nationally, to almost 14,000 after the local process.
A CCG spokesman said the local process was a combination of “working through the GP patient lists with our primary care patient coordination service (these are additional staff in primary care that coordinate patient care pathways) and local GP knowledge of individual patients.” Other parts of London have some of the lowest proportions of the population on the shielding list, such as Tower Hamlets, with 2.6 per cent.
NHS Digital has recently published the
data on local shielding lists to inform the public and “support the health and social care system in planning”. The national list currently stands at around 2.2 million, an increase of less than two-fold on that initially compiled centrally.
One CCG chief, who asked not to be named, described the process as “a mess” due to the speed in which GPs were told to compile the lists, as well as unclear guidance from the centre. Another said there had been issues with different areas having different clinical systems, and the absence of fixed codes to record certain conditions.
Rosie Cooper MP, who has previously been critical of the process, said the variation was “very worrying”, as it suggests some patients could be denied support. She added: “The communication of the rules were abysmal. I have spoken to GPs who were completely bemused and thought there was a very narrow list of specific illnesses, by which I mean that they thought it was only specific cancers which qualified.”
Dr Graham Jackson, chair of NHS Clinical Commissioners, said: “The process to identify patients to be shielded seems to have been a mixed bag for our member CCGs. We know that some CCGs and commissioning support units have led on this process, but in many areas it has been led by general practices.”
NHS England did not respond to questions about whether the variation was accepted, or whether there would be further work with outliers to review their lists. A spokeswoman said: “To ensure accuracy and completeness, GPs and specialists were asked to review the NHS shielded patient list as identified by the national algorithm, and use their clinical judgement to add or remove patients as appropriate.”
Dr Nikki Kanani, NHS England’s director of primary care,
has previously apologised to GPs about “frustrating” elements of the processes used to build the lists, including the tight timelines that were required.
The
guidance for shielding patients was relaxed slightly earlier this month, and is expected to be extended next week.