Ebbing Strength, Fading Power: Unveiling the Impact of Persistent Fatigue on Muscle Performance in COVID-19 Survivors
Kowal, Mateusz; Morgiel, Ewa; Winiarski, Sławomir; Dymarek, Robert; Bajer, Weronika; Madej, Marta; Sebastian, Agata; Madziarski, Marcin; Wedel, Nicole; Proc, Krzysztof; Madziarska, Katarzyna; Wiland, Piotr; Paprocka-Borowicz, Małgorzata
The total number of confirmed cases of COVID-19 caused by SARS-CoV-2 virus infection is over 621 million. Post-COVID-19 syndrome, also known as long COVID or long-haul COVID, refers to a persistent condition where individuals experience symptoms and health issues after the acute phase of COVID-19. The aim of this study was to assess the strength and fatigue of skeletal muscles in people recovered from COVID-19.
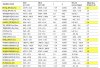
A total of 94 individuals took part in this cross-sectional study, with 45 participants (referred to as the Post-COVID Cohort, PCC) and 49 healthy age-matched volunteers (Healthy Control Cohort, HCC). This research article uses the direct dynamometry method to provide a detailed analysis of post-COVID survivors’ strength and power characteristics. The Biodex System 4 Pro was utilized to evaluate muscle strength characteristics during the fatigue test.
The fatigue work in extensors and flexors was significantly higher in the PCC. The PCC also showed significantly less power in both extensors and flexors compared to the HCC.
In conclusion, this study provides compelling evidence of the impact of post-COVID-19 fatigue on muscle performance, highlighting the importance of considering these effects in the rehabilitation and care of individuals recovering from the virus. PCC achieved lower muscle strength values than HCC.
Link | PDF (Sensors) [Open Access]
Kowal, Mateusz; Morgiel, Ewa; Winiarski, Sławomir; Dymarek, Robert; Bajer, Weronika; Madej, Marta; Sebastian, Agata; Madziarski, Marcin; Wedel, Nicole; Proc, Krzysztof; Madziarska, Katarzyna; Wiland, Piotr; Paprocka-Borowicz, Małgorzata
The total number of confirmed cases of COVID-19 caused by SARS-CoV-2 virus infection is over 621 million. Post-COVID-19 syndrome, also known as long COVID or long-haul COVID, refers to a persistent condition where individuals experience symptoms and health issues after the acute phase of COVID-19. The aim of this study was to assess the strength and fatigue of skeletal muscles in people recovered from COVID-19.
A total of 94 individuals took part in this cross-sectional study, with 45 participants (referred to as the Post-COVID Cohort, PCC) and 49 healthy age-matched volunteers (Healthy Control Cohort, HCC). This research article uses the direct dynamometry method to provide a detailed analysis of post-COVID survivors’ strength and power characteristics. The Biodex System 4 Pro was utilized to evaluate muscle strength characteristics during the fatigue test.
The fatigue work in extensors and flexors was significantly higher in the PCC. The PCC also showed significantly less power in both extensors and flexors compared to the HCC.
In conclusion, this study provides compelling evidence of the impact of post-COVID-19 fatigue on muscle performance, highlighting the importance of considering these effects in the rehabilitation and care of individuals recovering from the virus. PCC achieved lower muscle strength values than HCC.
Link | PDF (Sensors) [Open Access]