Kalliope
Senior Member (Voting Rights)
Transl Med
Endothelial dysfunction and altered endothelial biomarkers in patients with post-COVID-19 syndrome and chronic fatigue syndrome (ME/CFS) Milan Haffke et al
Abstract
Background: Fatigue, exertion intolerance and post-exertional malaise are among the most frequent symptoms of Post-COVID Syndrome (PCS), with a subset of patients fulfilling criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). As SARS-CoV-2 infects endothelial cells, causing endotheliitis and damaging the endothelium, we investigated endothelial dysfunction (ED) and endothelial biomarkers in patients with PCS.
Methods: We studied the endothelial function in 30 PCS patients with persistent fatigue and exertion intolerance as well as in 15 age- and sex matched seronegative healthy controls (HCs). 14 patients fulfilled the diagnostic criteria for ME/CFS. The other patients were considered to have PCS. Peripheral endothelial function was assessed by the reactive hyperaemia index (RHI) using peripheral arterial tonometry (PAT) in patients and HCs. In a larger cohort of patients and HCs, including post-COVID reconvalescents (PCHCs), Endothelin-1 (ET-1), Angiopoietin-2 (Ang-2), Endocan (ESM-1), IL-8, Angiotensin-Converting Enzyme (ACE) and ACE2 were analysed as endothelial biomarkers.
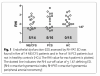
Results: Five of the 14 post-COVID ME/CFS patients and five of the 16 PCS patients showed ED defined by a diminished RHI (< 1.67), but none of HCs exhibited this finding. A paradoxical positive correlation of RHI with age, blood pressure and BMI was found in PCS but not ME/CFS patients. The ET-1 concentration was significantly elevated in both ME/CFS and PCS patients compared to HCs and PCHCs. The serum Ang-2 concentration was lower in both PCS patients and PCHCs compared to HCs.
Conclusion: A subset of PCS patients display evidence for ED shown by a diminished RHI and altered endothelial biomarkers. Different associations of the RHI with clinical parameters as well as varying biomarker profiles may suggest distinct pathomechanisms among patient subgroups.
Endothelial dysfunction and altered endothelial biomarkers in patients with post-COVID-19 syndrome and chronic fatigue syndrome (ME/CFS) Milan Haffke et al
Abstract
Background: Fatigue, exertion intolerance and post-exertional malaise are among the most frequent symptoms of Post-COVID Syndrome (PCS), with a subset of patients fulfilling criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). As SARS-CoV-2 infects endothelial cells, causing endotheliitis and damaging the endothelium, we investigated endothelial dysfunction (ED) and endothelial biomarkers in patients with PCS.
Methods: We studied the endothelial function in 30 PCS patients with persistent fatigue and exertion intolerance as well as in 15 age- and sex matched seronegative healthy controls (HCs). 14 patients fulfilled the diagnostic criteria for ME/CFS. The other patients were considered to have PCS. Peripheral endothelial function was assessed by the reactive hyperaemia index (RHI) using peripheral arterial tonometry (PAT) in patients and HCs. In a larger cohort of patients and HCs, including post-COVID reconvalescents (PCHCs), Endothelin-1 (ET-1), Angiopoietin-2 (Ang-2), Endocan (ESM-1), IL-8, Angiotensin-Converting Enzyme (ACE) and ACE2 were analysed as endothelial biomarkers.
Results: Five of the 14 post-COVID ME/CFS patients and five of the 16 PCS patients showed ED defined by a diminished RHI (< 1.67), but none of HCs exhibited this finding. A paradoxical positive correlation of RHI with age, blood pressure and BMI was found in PCS but not ME/CFS patients. The ET-1 concentration was significantly elevated in both ME/CFS and PCS patients compared to HCs and PCHCs. The serum Ang-2 concentration was lower in both PCS patients and PCHCs compared to HCs.
Conclusion: A subset of PCS patients display evidence for ED shown by a diminished RHI and altered endothelial biomarkers. Different associations of the RHI with clinical parameters as well as varying biomarker profiles may suggest distinct pathomechanisms among patient subgroups.