We have replicated data relating to association with EBV and several other infections. We have what looks like a reliable estimate of genetic causation (~10%), with replication other than in one or two outlying studies.
Responding to this from another thread.
Relevant part of DecodeME paper:
We estimated ME/CFS SNP-based heritability from GWAS-1, based on the LDSC method and reported on a liability scale. It was modest but significantly different from zero, with ℎ 2 = 0.095 (SD = 0.006).
So my understanding is that SNP-based heritability, as reported above, only captures the genetic influence from what was measured in the study: common variants. That means it misses any genetic influence of rare variants. And I don't think it captures structural changes like copy number variants and inversions.
Also, I think GWAS tests assume a certain model, which I think is most commonly the additive model, meaning having one copy of the risk allele increases risk by some amount and having two alleles doubles the risk. As opposed to a dominance model, where having one or two alleles causes equal increases in risk, or a recessive model, where only having both risk alleles can increase risk.
Regenie documentation says you can choose the model to use. If you set it to additive, I think you would miss a lot of the influence from recessive or dominant mutations.
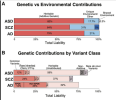
Here is an image from a paper visualizing the genetic contributions to autism spectrum disorder (ASD), schizophrenia (SCZ), and Alzheimer's disease (AD). For autism, for example, the genetic heritability is estimated at 82% of total liability (liability includes genetic and environmental influences). Yet the portion based on common variants is only around 12%. There's also some heritability due to rare variants, non-additive variants, plus 59% of liability is genetic heritability which has not been attributed to a specific factor.
From variants to mechanisms: Neurogenomics in the post-GWAS era, 2025, Neuron
I think total genetic heritability will be better captured by family studies, though I'm not sure how exactly they disentangle shared environment.