Sly Saint
Senior Member (Voting Rights)
interesting thread from Keith Geraghty
Given I could not get an appointment at my GP today, and have seen patients in tears at the desk and the reception staff told me they have to turn away most patients most days, I asked myself..."who owns and runs my local GP practice?"......here is what I found..............
1. the Care Qual Commission give my local GP practice a good rating for all scores, incl responsiveness! I had assumed the practice was run by a Dr Astles - it is back in Leicester home area. https://cqc.org.uk/location/1-559578647 - but is now Willowbrook
2. The practice manager is a very senior person, a GP, Professor, doctor and holder of many positions and directorships of many private companies - His name is on public record as Professor Rishabh Prasad.
3. here is a
@reachleicester
newspaper article on a story re a patient who could not get an app. back in 2019 (pre-covid) & interview with Dr. Prasad - about how he was aware patients were struggling to get appointments.
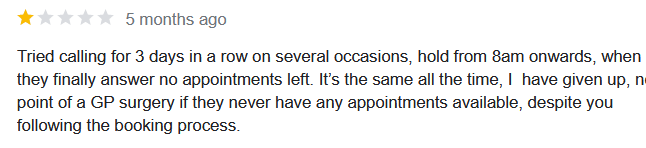
leicestermercury.co.uk
GP explains why patient at surgery struggle to see a doctor
'When we become GPs we do so to care for people, not to run efficient businesses'
4. My practice manager has a public record searchable as a
@HealthFdn
scholar & holds or held senior roles as Clinical Director at Digital Health Evaluation Services overseeing hundreds of millions of pounds budget for primary care services in the East Midlands region.
5. On public records I see my practice manager is actually Chairman Of The Board of 'Willows Health' who it seems may have control of my local GP practice, via ownership or management - it is hard to tell. So who are Willows Health? >
willowshealthcare.org
HOME | Willows Health
6. so just a recap: my local Dr GP practice is now Willowbrook, which is owned by Willows Health, with manager not onsite, Chair of a Company, multi-roled, multi-directorships. Ok - context, no appointments, patients unhappy, I'm still trying to understand who owns my GP?
Ok so Willows Health - "the Gold Standard for Care"? um really? Patients in tears, low quality ratings, awful comments about poor service and lack of appointments...who is deciding whats the Gold Standard here.
7. Mergers - private companies and Willows Health - why does this matter at all? Well its seems Willows owns more than one practice and patients are having to phone in from all practice areas in the morning at 8 am to fight for an appointment, all patients calling one phone line!
8. What Willows Health say their patients say about their care provision ....? Note the multiple practice locations
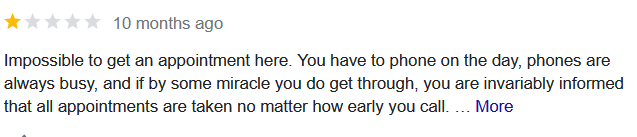
9. How patients rating Willowbrook, under Willows Health & patient feedback on google reviews "impossible to get an appointment here" & comments on Willows Medical Centre. Seems to me a consistent issue of complaint with lack of access to appointments and 8 am phone-in for all!
10. Willows Health is a Consortium of 10 GP practices owned/run by a private company. As a patient you have to phone at 8 am and most callers will not get an appointment - privatisation of this kind has implications for patient care, like me this morning & many others........
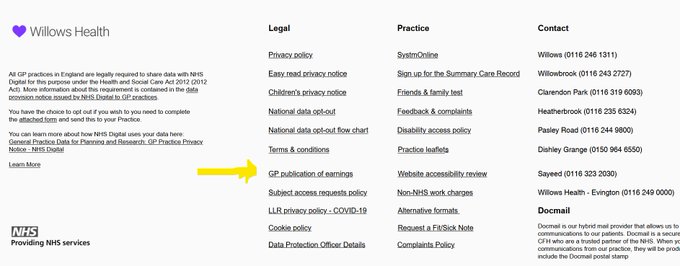
11. More from my search to understand who owns my home GP practice - to find out why its so difficult to get an appointment: looking at the consortium page the GP salaries link says across most of the 10 practice they only have 1 full-time GP salaried, https://willowshealthcare.org