nataliezzz
Senior Member (Voting Rights)
Obstructive sleep apnoea and quality of life in Ehlers-Danlos syndrome: A parallel cohort study
Thomas Gaisl, Cecilia Giunta, Daniel J Bratton, Kate Sutherland, Christian Schlatzer, Noriane Sievi, Daniel Franzen, Peter A Cistulli, Marianne Rohrbach, Malcolm Kohler
https://www.researchgate.net/publication/312232373_Obstructive_sleep_apnoea_and_quality_of_life_in_Ehlers-Danlos_syndrome_A_parallel_cohort_study (PDF available)
Abstract
Background: Patients with the connective tissue disorder Ehlers-Danlos syndrome (EDS) often suffer from fatigue, excessive daytime sleepiness and impaired quality of life. Obstructive sleep apnoea (OSA) may be an underlying cause for these symptoms but its prevalence in this population is unclear.
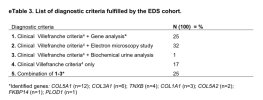
Methods: In this prospective parallel-cohort study, we included 100 adult patients with EDS (46% hypermobile-type, 35% classical-type and 19% other), which were one-to-one matched to 100 healthy adult controls according to sex, age, weight and height. Participants underwent structured interviews (including short-form 36) and level-3 respiratory polygraphy. OSA was defined as apnoea-hypopnea index ≥5/hour. Photographic craniofacial phenotyping was conducted in a subgroup. Conditional logistic regression was used to compare the prevalence of OSA.
Results: In patients with EDS, OSA prevalence was 32% versus 6% in the matched control group (OR 5.3 (95% CI 2.5 to 11.2); p<0.001). The EDS group reported impaired quality of life in all dimensions (p<0.05) and significantly higher excessive daytime sleepiness measured by the Epworth Sleepiness Scale (median (quartiles) 11 (7-14) vs 7 (5-10); p<0.001). OSA severity was positively associated with daytime sleepiness and lower quality of life in the EDS group. There was no evidence of a difference between the two study groups in terms of craniofacial phenotypes.
Conclusions: The prevalence of OSA is higher in patients with EDS than in a matched control group. This is of clinical relevance as it is associated with fatigue, excessive daytime sleepiness and impaired quality of life. Further studies are needed to assess the clinical benefit of OSA treatment in patients with EDS.
Thomas Gaisl, Cecilia Giunta, Daniel J Bratton, Kate Sutherland, Christian Schlatzer, Noriane Sievi, Daniel Franzen, Peter A Cistulli, Marianne Rohrbach, Malcolm Kohler
https://www.researchgate.net/publication/312232373_Obstructive_sleep_apnoea_and_quality_of_life_in_Ehlers-Danlos_syndrome_A_parallel_cohort_study (PDF available)
Abstract
Background: Patients with the connective tissue disorder Ehlers-Danlos syndrome (EDS) often suffer from fatigue, excessive daytime sleepiness and impaired quality of life. Obstructive sleep apnoea (OSA) may be an underlying cause for these symptoms but its prevalence in this population is unclear.
Methods: In this prospective parallel-cohort study, we included 100 adult patients with EDS (46% hypermobile-type, 35% classical-type and 19% other), which were one-to-one matched to 100 healthy adult controls according to sex, age, weight and height. Participants underwent structured interviews (including short-form 36) and level-3 respiratory polygraphy. OSA was defined as apnoea-hypopnea index ≥5/hour. Photographic craniofacial phenotyping was conducted in a subgroup. Conditional logistic regression was used to compare the prevalence of OSA.
Results: In patients with EDS, OSA prevalence was 32% versus 6% in the matched control group (OR 5.3 (95% CI 2.5 to 11.2); p<0.001). The EDS group reported impaired quality of life in all dimensions (p<0.05) and significantly higher excessive daytime sleepiness measured by the Epworth Sleepiness Scale (median (quartiles) 11 (7-14) vs 7 (5-10); p<0.001). OSA severity was positively associated with daytime sleepiness and lower quality of life in the EDS group. There was no evidence of a difference between the two study groups in terms of craniofacial phenotypes.
Conclusions: The prevalence of OSA is higher in patients with EDS than in a matched control group. This is of clinical relevance as it is associated with fatigue, excessive daytime sleepiness and impaired quality of life. Further studies are needed to assess the clinical benefit of OSA treatment in patients with EDS.