Dolphin
Senior Member (Voting Rights)
https://journals.physiology.org/doi/abs/10.1152/ajpregu.00071.2024
Research Article
Phenylephrine Alters Phase Synchronization between Cerebral Blood Velocity and Blood Pressure in Chronic Fatigue Syndrome with Orthostatic Intolerance
Marvin S. Medow* and Julian M. Stewart
29 APR 2024https://doi.org/10.1152/ajpregu.00071.2024
Abstract
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) with orthostatic intolerance (OI) is characterized by neuro-cognitive deficits perhaps related to upright hypocapnia and loss of cerebral autoregulation (CA).
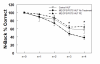
We performed N-back neurocognition testing and calculated the phase synchronization index (PhSI) between Arterial Pressure (AP) and cerebral blood velocity (CBV) as a time-dependent measurement of cerebral autoregulation in 11 control (mean age=24.1 years) and 15 ME/CFS patients (mean age=21.8 years).
All ME/CFS patients had postural tachycardia syndrome (POTS).
A 10-minute 60⁰ head-up tilt (HUT) significantly increased heart rate (109.4 ± 3.9 vs. 77.2 ± 1.6 beats/min, P <0.05) and respiratory rate (20.9 ± 1.7 vs. 14.2 ± 1.2 breaths/min, P < 0.05) and decreased end-tidal CO2 (ETCO2; 33.9 ± 1.1 vs. 42.8 ± 1.2 Torr, P < 0.05) in ME/CFS vs. control.
In ME/CFS, HUT significantly decreased CBV compared to control (-22.5% vs -8.7%, p<0.005).
To mitigate the orthostatic CBV reduction, we administered supplemental CO2, phenylephrine and acetazolamide and performed N-back testing supine and during HUT.
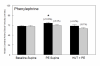
Only phenylephrine corrected the orthostatic decrease in neurocognition by reverting % correct n=4 N-back during HUT in ME/CFS similar to control (ME/CFS=38.5±5.5 vs. ME/CFS+PE= 65.6±5.7 vs. Control 56.9±7.5).
HUT in ME/CFS resulted in increased PhSI values indicating decreased CA.
While CO2 and Acetazolamide had no effect on PhSI in ME/CFS, PE caused a significant reduction in PhSI (ME/CFS=0.80±0.03 vs ME/CFS+PE= 0.69±0.04, p< 0.05) and improved cerebral autoregulation.
Thus, PE improved neurocognitive function in ME/CFS patients, perhaps related to improved neurovascular coupling, cerebral autoregulation and maintenance of CBV.
Citation:
Phenylephrine Alters Phase Synchronization between Cerebral Blood Velocity and Blood Pressure in Chronic Fatigue Syndrome with Orthostatic Intolerance
Marvin S. Medow and Julian M. Stewart
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology 0 0:0
Grants and funding
Research Article
Phenylephrine Alters Phase Synchronization between Cerebral Blood Velocity and Blood Pressure in Chronic Fatigue Syndrome with Orthostatic Intolerance
Marvin S. Medow* and Julian M. Stewart
29 APR 2024https://doi.org/10.1152/ajpregu.00071.2024
Abstract
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) with orthostatic intolerance (OI) is characterized by neuro-cognitive deficits perhaps related to upright hypocapnia and loss of cerebral autoregulation (CA).
We performed N-back neurocognition testing and calculated the phase synchronization index (PhSI) between Arterial Pressure (AP) and cerebral blood velocity (CBV) as a time-dependent measurement of cerebral autoregulation in 11 control (mean age=24.1 years) and 15 ME/CFS patients (mean age=21.8 years).
All ME/CFS patients had postural tachycardia syndrome (POTS).
A 10-minute 60⁰ head-up tilt (HUT) significantly increased heart rate (109.4 ± 3.9 vs. 77.2 ± 1.6 beats/min, P <0.05) and respiratory rate (20.9 ± 1.7 vs. 14.2 ± 1.2 breaths/min, P < 0.05) and decreased end-tidal CO2 (ETCO2; 33.9 ± 1.1 vs. 42.8 ± 1.2 Torr, P < 0.05) in ME/CFS vs. control.
In ME/CFS, HUT significantly decreased CBV compared to control (-22.5% vs -8.7%, p<0.005).
To mitigate the orthostatic CBV reduction, we administered supplemental CO2, phenylephrine and acetazolamide and performed N-back testing supine and during HUT.
Only phenylephrine corrected the orthostatic decrease in neurocognition by reverting % correct n=4 N-back during HUT in ME/CFS similar to control (ME/CFS=38.5±5.5 vs. ME/CFS+PE= 65.6±5.7 vs. Control 56.9±7.5).
HUT in ME/CFS resulted in increased PhSI values indicating decreased CA.
While CO2 and Acetazolamide had no effect on PhSI in ME/CFS, PE caused a significant reduction in PhSI (ME/CFS=0.80±0.03 vs ME/CFS+PE= 0.69±0.04, p< 0.05) and improved cerebral autoregulation.
Thus, PE improved neurocognitive function in ME/CFS patients, perhaps related to improved neurovascular coupling, cerebral autoregulation and maintenance of CBV.
Citation:
Phenylephrine Alters Phase Synchronization between Cerebral Blood Velocity and Blood Pressure in Chronic Fatigue Syndrome with Orthostatic Intolerance
Marvin S. Medow and Julian M. Stewart
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology 0 0:0
Grants and funding
- RO1 HL 112736/HHS | NIH | National Heart, Lung, and Blood Institute (NHLBI)
- RO1 HL 074873/HHS | NIH | National Heart, Lung, and Blood Institute (NHLBI)
- 1R56HL162752/HHS | NIH | National Heart, Lung, and Blood Institute (NHLBI)
- Solve ME/CFS Initiative (SMCI)
Last edited: