Now on Youtube:
00:00 Amy Proal–An overview of PolyBio’s complex chronic illness research & clinical trials program
10:35 Resia Pretorius–Heterogenous fibrinaloid complexes (microclots): characterizing different phenotypes
19:46 Mark Painter–T cells as biosensors of viral persistence in Long COVID
32:05 David Price–Infectious, immune, and microbiome signals in the long COVID lung
44:39 Johan Van Wyenburgh–A real-world prospective study of antiviral and anticoagulant use in Long COVID
56:24 Q&A (Painter--What are the current pathways to get the Wherry Lab's T cell biosensor technology into the clinic?)
59:16 Michael Peluso–SARS-CoV-2 monoclonal antibodies in long COVID: Key findings and future directions
1:14:52 Nadia Roan—Phenotypic features of CD8+ T cells specific for SARS-CoV-2 and herpesviruses in people with and without Long COVID
1:26:47 Lael Yonker–Long COVID gut barrier permeability and neutrophil/clotting/spike interactions
1:40:58 Chris Dupont–An update on the Tissue Analysis Pipeline: a focus on craniocervical ligament
1:46:50 Gene Tan–Deep Characterization of antiviral immune responses and long COVID pathogenesis
1:58:01 Marcelo Freire–Analysis of small fiber neuropathy punch biopsy and other tissue samples via spatial transcriptomics
2:10:17 Michael VanElzakker–A study of the neuroimmune basis of brainfog symptoms
2:21:54 Francis Eun Lee–Use of MENSA to identify an immune snapshot for SARS-CoV-2 persistence and herpesvirus reactivation in Long COVID
2:35:08 Timothy Henrich–Molecular imaging in long COVID, plus tissue biopsy project updates
2:46:15 Huaitao Cheng–Uncovering mucosal immune dysregulation in long COVID patients with gastrointestinal symptoms
2:55:32 Akiko Iwasaki–Uncovering mucosal immune dysregulation in long COVID patients with gastrointestinal symptom
3:05:19 Victoria Cortes Bastos–Cerebrospinal fluid and plasma phenotyping reveals distinct subgroups of ME/CFS
3:15:49 Mario Murakami–Ultrahigh resolution neuroimaging shows neuroimmune sensitization across infection-associated chronic conditions
3:25:32 Sara Cherry–Long COVID: Defining viral RNA reservoirs in the gastrointestinal tract
3:35:08 Saurabh Mehandru–Investigating the role of SARS-CoV-2 gastrointestinal tract persistence in Long COVID pathogenesis
3:48:40 Q&A (VanElzkker–What are your thoughts on treatment for vagus nerve neuroimmune signalling? And which medications have vagus nerve innervation activity?)
3:51:26 Esen Sefik–A humanized mouse model of SARS-COV-2 RNA persistence
4:01:34 Melanie Walker–Characterization of the vagus nerve microbiome/virome
4:12:41 Steven Deeks–The Reservoir Assay Validation and Evaluation Network (RAVEN) as a model to inform SARS-CoV-2 reservoir diagnostics
4:22:15 Shannon Delaney–The Reservoir Assay Validation and Evaluation Network (RAVEN) as a model to inform SARS-CoV-2 reservoir diagnostics
4:33:04 Shannon Stott–Microfluidics capture of SARS-CoV-2 particles in long COVID blood
4:44:06 Q & A (Proal–What efforts are being done to address Post-Vaccine symptoms for COVID-19?; Differentiating Spike protein from COVID infection versus vaccine; Delaney–Medical Diagnostics lab for Bartonella testing; Walker–Can bacteria infect the vagus nerve?)
4:50:01 Daniel Izquierdo Garcia–Evaluation of tissue fibrin accumulation in long COVID via PET imaging & blood analysis
5:01:33 David Putrino–Update overview of Long COVID, Lyme+ and other CoRE clinical trials
5:17:13 Silvia Lage–Persistent immune dysregulation and metabolic alterations following SARS-CoV-2 infection
5:27:15 Zian Tseng–The COVID POST SCD (POstmortem Systematic invesTigation of Sudden Cardiac Death) Study
5:39:52 Benjamin Readhead–Validation of a Cytomegalovirus-based biomarker for Alzheimer's disease
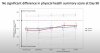
5:52:53 Max Qian –Long COVID endotype identification
6:06:18 Daniel Chertow–Overview of new NIH long COVID tissue biopsy trial
6:16:50 Amy Proal discusses NIH trial participation, thank-you to IACI community