Andy
Senior Member (Voting rights)
Recurrent abdominal pain (RAP) is a common medically unexplained symptom among children worldwide. However, the biological mechanisms behind the development of functional and behavioral symptoms and changes in blood markers have not been well explored.
This study aimed to assess changes in the concentrations of inflammatory markers, including cytokines and tryptophan catabolites, in the serum of children with RAP compared to those with subclinical infections. Children with RAP but without organic diseases were included, and those with asymptomatic intestinal parasitic infections were used as a subclinical infection cohort. Blood samples were collected and used to measure the cytokine profile using Multiplex Immunoassay and tryptophan catabolites using high performance liquid chromatography.
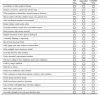
Children with RAP showed significantly higher concentrations of serum tumor necrotic factor-α, p<0.05, but lower concentrations of IL-10, p<0.001, IL-6, p<0.001 and brain-derived neurotrophic factors (BDNF) p<0.01. In addition, a significant increase in the metabolite of the kynurenine pathway, 3-hydroxyanthranilic acid (3-HAA) p<0.01, a significant decrease in the concentrations of anthranilic acid (AA) p<0.001, together with an increased ratio of serum 3-HAA to AA (3-HAA/AA) p<0.001, was found in this cohort.
These findings indicate the significant activation of the immune system and presence of inflammation in children with RAP than those with subclinical parasitic infections. Moreover, children with RAP tested with the Strengths and Difficulties Questionnaire (SDQ), displayed high psychological problems though these SDQ scores were not statistically associated with measured cytokines and kynurenine metabolites.
We however could hypothesize that the pro-inflammatory state together with concomitant low concentrations of BDNF in those children with RAP could play a role in psychological stress and experiencing medically unexplained symptoms.
Open access, https://www.frontiersin.org/articles/10.3389/fimmu.2021.702301/full
This study aimed to assess changes in the concentrations of inflammatory markers, including cytokines and tryptophan catabolites, in the serum of children with RAP compared to those with subclinical infections. Children with RAP but without organic diseases were included, and those with asymptomatic intestinal parasitic infections were used as a subclinical infection cohort. Blood samples were collected and used to measure the cytokine profile using Multiplex Immunoassay and tryptophan catabolites using high performance liquid chromatography.
Children with RAP showed significantly higher concentrations of serum tumor necrotic factor-α, p<0.05, but lower concentrations of IL-10, p<0.001, IL-6, p<0.001 and brain-derived neurotrophic factors (BDNF) p<0.01. In addition, a significant increase in the metabolite of the kynurenine pathway, 3-hydroxyanthranilic acid (3-HAA) p<0.01, a significant decrease in the concentrations of anthranilic acid (AA) p<0.001, together with an increased ratio of serum 3-HAA to AA (3-HAA/AA) p<0.001, was found in this cohort.
These findings indicate the significant activation of the immune system and presence of inflammation in children with RAP than those with subclinical parasitic infections. Moreover, children with RAP tested with the Strengths and Difficulties Questionnaire (SDQ), displayed high psychological problems though these SDQ scores were not statistically associated with measured cytokines and kynurenine metabolites.
We however could hypothesize that the pro-inflammatory state together with concomitant low concentrations of BDNF in those children with RAP could play a role in psychological stress and experiencing medically unexplained symptoms.
Open access, https://www.frontiersin.org/articles/10.3389/fimmu.2021.702301/full