The evidence is moderately strong that something in the blood is large molecule size, which might include vesicles, and mediates cellular energy deficit. It may or may not be the whole problem, but it must indeed be caused by something. As a possible mediating mechanism its a target for treatment. If its not causal then it probably wont directly lead to a cure, but it might point the way.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Ron Davis latest: more evidence of "something in the blood" (Simon M blog)
Mij
Senior Member (Voting Rights)
I read a study (can't find it right now) that increased lactate impairs the coagulation system. I had an ISAC panel done years ago from HEMEX labs, and one particular marker indicated 'something in the blood'- interestingly enough. My doctor travelled down to a workshop in Arizona to meet with physicians and David Berg (lab owner) and he was very insistent that it was a virus. The virologist and head haematologist disagreed.
I don't know whether I should have posted this on the lactate thread or this one.
I don't know whether I should have posted this on the lactate thread or this one.
MeSci
Senior Member (Voting Rights)
I did an internet search for "increased lactate impairs coagulation" and got this:I read a study (can't find it right now) that increased lactate impairs the coagulation system. I had an ISAC panel done years ago from HEMEX labs, and one particular marker indicated 'something in the blood'- interestingly enough. My doctor travelled down to a workshop in Arizona to meet with physicians and David Berg (lab owner) and he was very insistent that it was a virus. The virologist and head haematologist disagreed.
I don't know whether I should have posted this on the lactate thread or this one.
https://journals.lww.com/jnsa/Abstr..._Lactate_Levels_Impair_the_Coagulation.7.aspx
and several others.
Simon M
Senior Member (Voting Rights)
Not an answer for ME/CFS, but here's an example of (non-nanoneedle) bioimpedance being used to measure changes in cells for studying the effect of candidate drugs in fibrotic disease.What do nanoneedle findings actually mean? How do we know that what happens in this test in vitro will be relevant to what happens in vivo?
https://pubs.acs.org/doi/full/10.1021/acssensors.7b00442?src=recsys#
Crucially, the study identified what was happening at the cellular level as bioimpedance changed.
Hopefully, one day we will have similar for mecfs.We confirmed the validity of the developed biochemical impedance biosensor as an tool for in vitro screening of antifibrotic compounds and provided quantitative information on subcellular influences of the examined chemical molecules using correlative microscopy analyses that monitor the average cell area, cell morphology, and the amount and directionality of the deposited extracellular matrix protein collagen and measurement of cytosolic Ca2+ changes.
Last edited:
Andy
Senior Member (Voting rights)
http://www.virology.ws/2019/12/16/t...grath-on-ron-davis-on-something-in-the-blood/Simon McGrath provides excellent accounts of research topics at his blog, ME/CFS Research Review. He is skilled at rendering complicated stuff into easy-to-understand prose. On December 10th, Simon posted this update of developments discussed by Stanford geneticist Ron Davis during a recent talk at the Albert Einstein College of Medicine in New York.
In his talk, Davis discussed the latest on the notion that “something in the blood” is playing a key role in the disease–a topic being explored by a number of research teams in addition to his. With Simon’s permission, I am re-posting his overview of the discussion. Since I am incapable of advanced technological maneuvers, I was delighted to find out that I could just copy Simon’s blog and paste it in here, and the graphics would reproduce here as they appeared there. Whew!
Barry
Senior Member (Voting Rights)
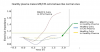
Surely there is something else significant about this graph, other than the very high value reached by the "ME/CFS Cells in CFS Plasma" line. The shape of the lines.
"Healthy Cells in Healthy Plasma" is the only line that is almost straight. The others have the same characteristic drop in impedance before then rising again, even though the timings and amplitudes are different. So any ME/CFS association would seem to be influencing healthy cells or healthy plasma. Is that dip not significant?
Last edited:
I have not had much sleep, so this may not be relevant at all.
Did healthy controls have IDO mutations ?
Graphs in CFS plasma remind me of the bistability " kick in "
Did experiment continue longer ( do we know of CFS in healthy plasma ever got to the same impedance level as HC?)
ETA what happens if data is logged?
Did healthy controls have IDO mutations ?
Graphs in CFS plasma remind me of the bistability " kick in "
Did experiment continue longer ( do we know of CFS in healthy plasma ever got to the same impedance level as HC?)
ETA what happens if data is logged?
lansbergen
Senior Member (Voting Rights)
Graphs in CFS plasma remind me of the bistability " kick in "
https://en.wikipedia.org/wiki/Bistability
In biological and chemical system
Bistability is key for understanding basic phenomena of cellular functioning, such as decision-making processes in cell cycle progression, cellular differentiation,[5] and apoptosis. It is also involved in loss of cellular homeostasis associated with early events in cancer onset and in prion diseases as well as in the origin of new species (speciation).[6]
Thanks. I feel a bucket load of coffee is needed to get any brain function today!https://en.wikipedia.org/wiki/Bistability
In biological and chemical system
Bistability is key for understanding basic phenomena of cellular functioning, such as decision-making processes in cell cycle progression, cellular differentiation,[5] and apoptosis. It is also involved in loss of cellular homeostasis associated with early events in cancer onset and in prion diseases as well as in the origin of new species (speciation).[6]
Snow Leopard
Senior Member (Voting Rights)
A simple hypothetical explanation for the cellular response to the salt challenge (in the nanoneedle study) is inhibited Na+/K+-ATPase activity (which is in turn upregulated by cAMP activity). Suggesting altered G protein coupled receptor activity, downregulation of Gs activity or upregulated Gi activity.
I have had an interest in this area for a long time, largely because of the cAMP/Ca++ axis, and resveratrol. One of the drugs under invesigation by RonDavis' group has a resveratrol version.which is in turn upregulated by cAMP activity
Regarding the thing in the blood, while I think it would be important to figure out exactly what it is, finding it wouldn't necessarily solve the puzzle. There was another thread about failed Alzheimer's research. The prevailing hypothesis used to be that amyloid beta was the factor that caused or at least served as a main driver to the disease, but from the latest understanding, it seems like amyloid plaques are probably better described as a consequence of the disease.
Using the Alzheimer's research analogy, it could be that the "something in the blood" finding isn't close to the actual root cause of ME/CFS. If that is the case, the next problematic is what is causing the factor in the blood to form, and so on. From thereon you may end up back to cytokines and the immune system and eventually you have completed the circle. So yeah, I'm not envying the task ahead of ME/CFS researchers.
I don't have specialist knowledge; however, Ron mentioned that it should be possible to:
- identify what the "something in the blood" is; and
- work back/upstream from the something in the blood i.e. to find where it is coming from (parent cells).
Potentially this requires separating plasma into fractions (nano-needle) and testing these. E.g. at it's simplest filtering out exosomes and testing these on a relatively high resolution mass spectrometer - to find candidates for "something in the blood" and possible sources for the exosomes - protein signature.
It may simply be a resource issues not a knowledge/technology issue.
I still hope that the something in the blood keeps being true, but i got a cycle of 7 plasma exchanges 2 months ago. Did absolutely nothing for me. Doesnt confirm or deny anything. Still i would have hoped for a change for the better if you believe its something in the plasma.
I gather there's been some comment on-line regarding "positive" results from Carmen Scheibenbogen's group --- "Immunoadsorption is an apheresis procedure to remove specific proteins from a patient’s plasma" [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5854315/]
Theory was they may have accidentally removed the "something in the blood". All conjecture of course!
If I remember right from @Andy's Q&A video with Karl Morten he said he would add an experiment to his wish list to look at cellular respiration using the same salt solution + plasma + cells to see if oxygen consumption differences can be seen.
I think Karl's really concerned to ensure they don't artificially create this effect. Remember how Ron's red blood cell deformability work de-railed temporarily, due to using buffer rather than plasma from people with ME --- So Karl want's to repeat his experiments in a way that replicates the real world scenario --- all very complex to me, so my explanation is poor!
It also could be the amount of something in the blood. There could be too little (or none) of something in the blood that's necessary, or too much of something that may or may not be necessary but which is toxic at high levels.
High on my list of suspects would be some metabolite created by a species of microbe in the gut - specifically deep in the small intestine where molecules are absorbed and it's hard to sample and study what's going on [just my personal speculation].
You and Derya Unutmaz?
@FMMM1 they did an Immunoadsorption which just removes the igG. So even if they wanted, i highly doubt they accidentally removed the something in the blood. Also i talked with some ppl from this study. Lets say it this way, the study seems not to reflect what they told me.
I got a cycle of 7 plasma exchanges in 10 days. Thats the most you can do in such a short time. And it did nothing.
I got a cycle of 7 plasma exchanges in 10 days. Thats the most you can do in such a short time. And it did nothing.
Forbin
Senior Member (Voting Rights)
You and Derya Unutmaz?
The general idea of CFS-like symptoms being created by the overgrowth of a toxin-producing microbe in the gut goes back at least to the early 1980's, with the "hangover" toxin acetaldehyde being thought overproduced by too much "candida albicans" in the gut.
The media played this up in the 1980's and "candida overgrowth" in the gut became considered a "fad" diagnosis by mainstream medicine. It would be pretty ironic if something along these lines turned out to be part of the puzzle.
Sly Saint
Senior Member (Voting Rights)
It might also be interesting if they could see whether the concentration of the 'something' changes up or down pre and post stressing; ie if there is a connection with PEM.It also could be the amount of something in the blood.
Hoopoe
Senior Member (Voting Rights)
The general idea of CFS-like symptoms being created by the overgrowth of a toxin-producing microbe in the gut goes back at least to the early 1980's, with the "hangover" toxin acetaldehyde being thought overproduced by too much "candida albicans" in the gut.
The media played this up in the 1980's and "candida overgrowth" in the gut became considered a "fad" diagnosis by mainstream medicine. It would be pretty ironic if something along these lines turned out to be part of the puzzle.
Dysbiosis could be quite plausibly be an exacerbating factor in the illness in some subgroup of patients.
Last edited:
well there goes SS31... https://www.biospace.com/article/stealth-bio-s-elamipretide-flunks-mitochondrial-myopathy-trial/
