nataliezzz
Senior Member (Voting Rights)
Somatic arousal and sleepiness/fatigue among patients with sleep-disordered breathing
Morris S. Gold, Tshering Amdo, Nadia Hasaneen and Avram R. Gold
https://www.researchgate.net/publication/289535169_Somatic_arousal_and_sleepinessfatigue_among_patients_with_sleep-disordered_breathing
Sci-Hub link to full paper: https://sci-hub.st/10.1007/s11325-015-1294-8
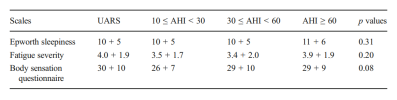
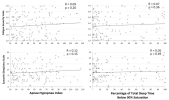
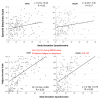
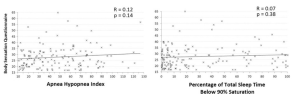
Methods: From 5 years of patient data, we obtained scores on the body sensation questionnaire (BSQ), measuring the level of SA, the fatigue severity scale (FSS), and Epworth sleepiness scale (ESS) for 152 consecutive UARS patients and 150 consecutive OSA/H patients. For each group, we correlated the FSS and ESS scores with the BSQ scores. Among the 45 UARS patients and 49 OSA/H patients treated with nasal CPAP who provided post-treatment data, we correlated change in FSS and ESS scores with change in BSQ scores.
Results: Scores on the BSQ, FSS, and ESS for UARS patients and OSA/H patients were comparable. In both UARS and OSA/H patients, both the FSS and ESS scores were positively correlated with the BSQ score. Nasal CPAP use decreased all three questionnaire scores in both patient groups. In the pooled data, changes in FSS were significantly correlated with changes in BSQ.
Conclusions: Our findings confirm our preliminary observations that sleepiness and fatigue among UARS patients are correlated with their level of SA and suggest that the same is true for OSA/H patients. The decrease of SA following treatment suggests that SDB is a cause of SA among patients with UARS and OSA/H.
Morris S. Gold, Tshering Amdo, Nadia Hasaneen and Avram R. Gold
https://www.researchgate.net/publication/289535169_Somatic_arousal_and_sleepinessfatigue_among_patients_with_sleep-disordered_breathing
Sci-Hub link to full paper: https://sci-hub.st/10.1007/s11325-015-1294-8
Abstract
Objectives: In a large clinical sample, we tested the hypothesis that levels of sleepiness and fatigue among upper airway resistance syndrome (UARS) patients are correlated with levels of somatic arousal (SA; reflecting the sympathetic nervous system component of the stress response). We also tested the correlations of post-treatment change in these three parameters, and we extended the investigation to obstructive sleep apnea/hypopnea (OSA/H) patients.Methods: From 5 years of patient data, we obtained scores on the body sensation questionnaire (BSQ), measuring the level of SA, the fatigue severity scale (FSS), and Epworth sleepiness scale (ESS) for 152 consecutive UARS patients and 150 consecutive OSA/H patients. For each group, we correlated the FSS and ESS scores with the BSQ scores. Among the 45 UARS patients and 49 OSA/H patients treated with nasal CPAP who provided post-treatment data, we correlated change in FSS and ESS scores with change in BSQ scores.
Results: Scores on the BSQ, FSS, and ESS for UARS patients and OSA/H patients were comparable. In both UARS and OSA/H patients, both the FSS and ESS scores were positively correlated with the BSQ score. Nasal CPAP use decreased all three questionnaire scores in both patient groups. In the pooled data, changes in FSS were significantly correlated with changes in BSQ.
Conclusions: Our findings confirm our preliminary observations that sleepiness and fatigue among UARS patients are correlated with their level of SA and suggest that the same is true for OSA/H patients. The decrease of SA following treatment suggests that SDB is a cause of SA among patients with UARS and OSA/H.