Andy
Senior Member (Voting rights)
Abstract
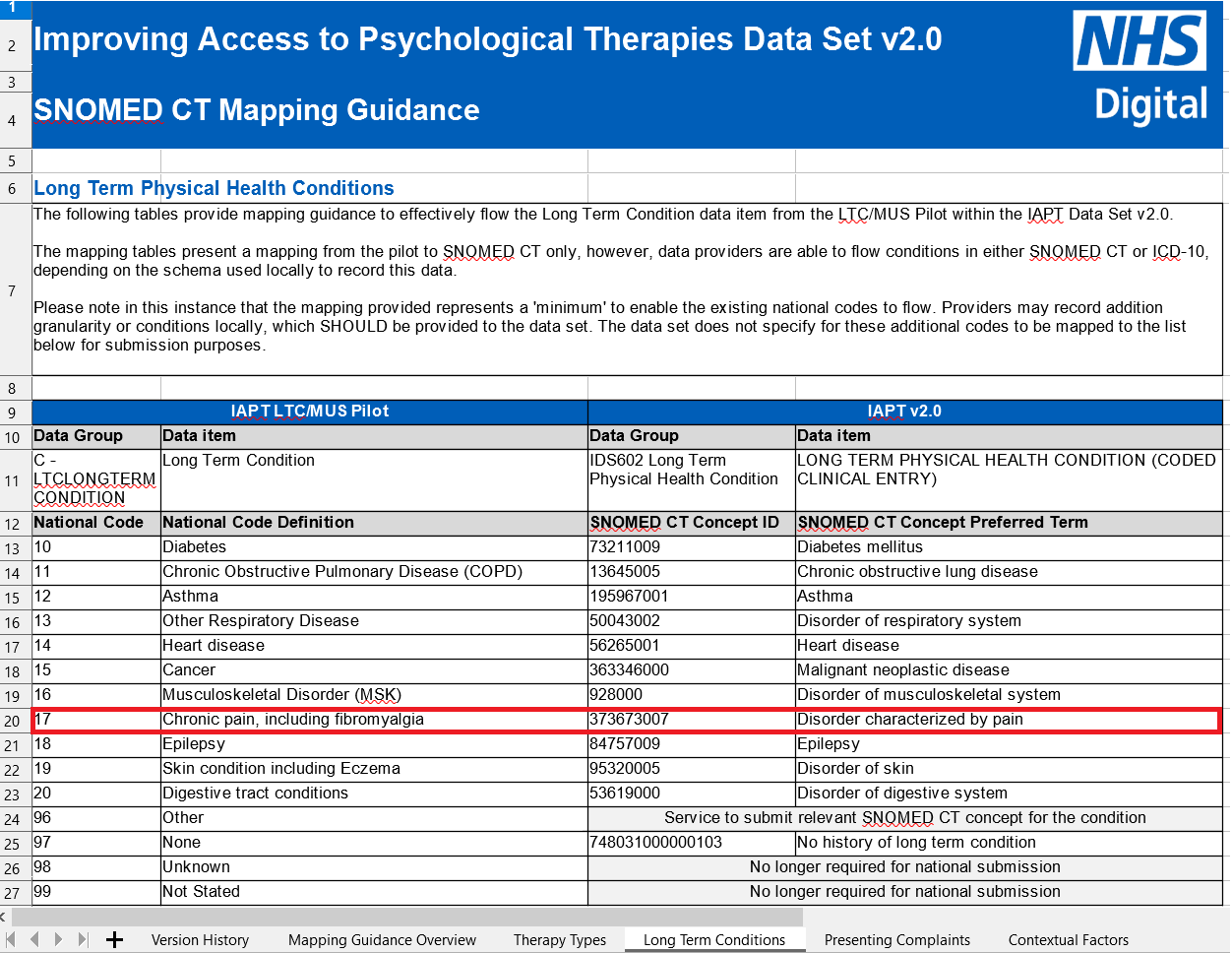
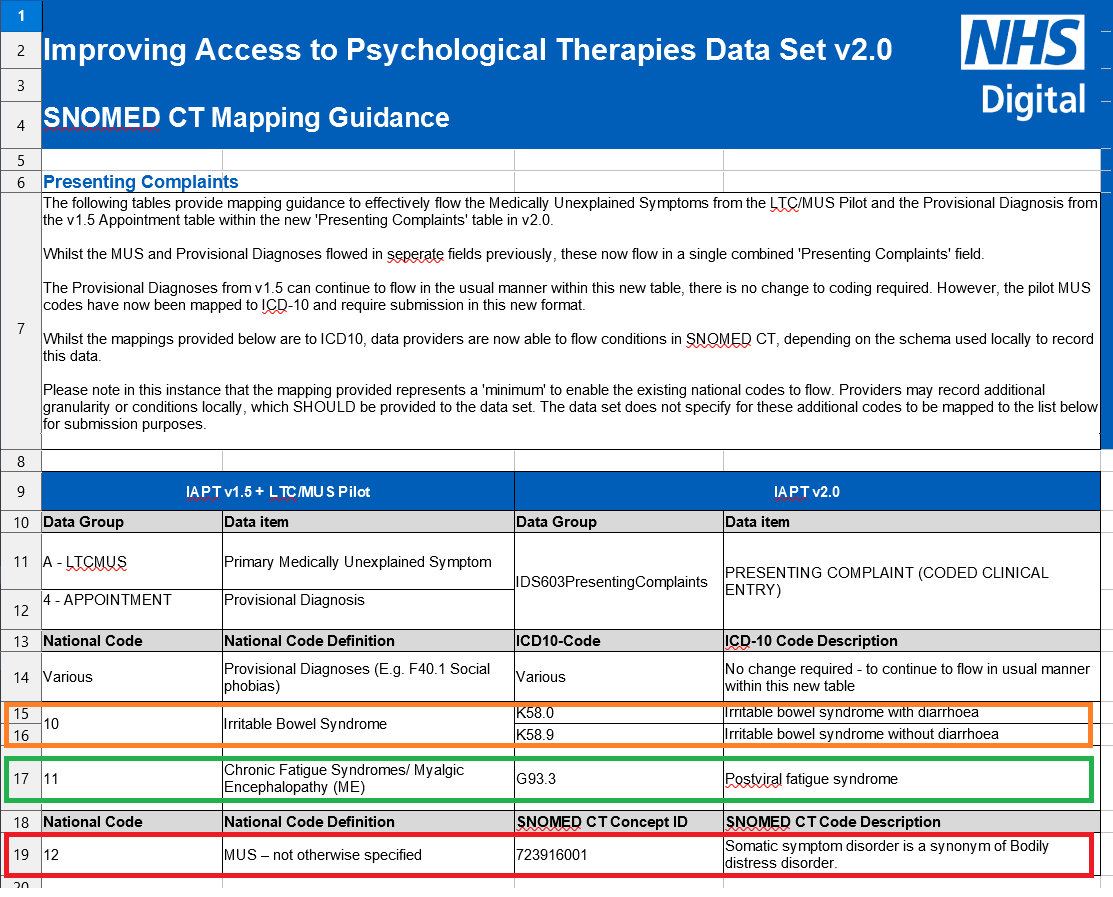
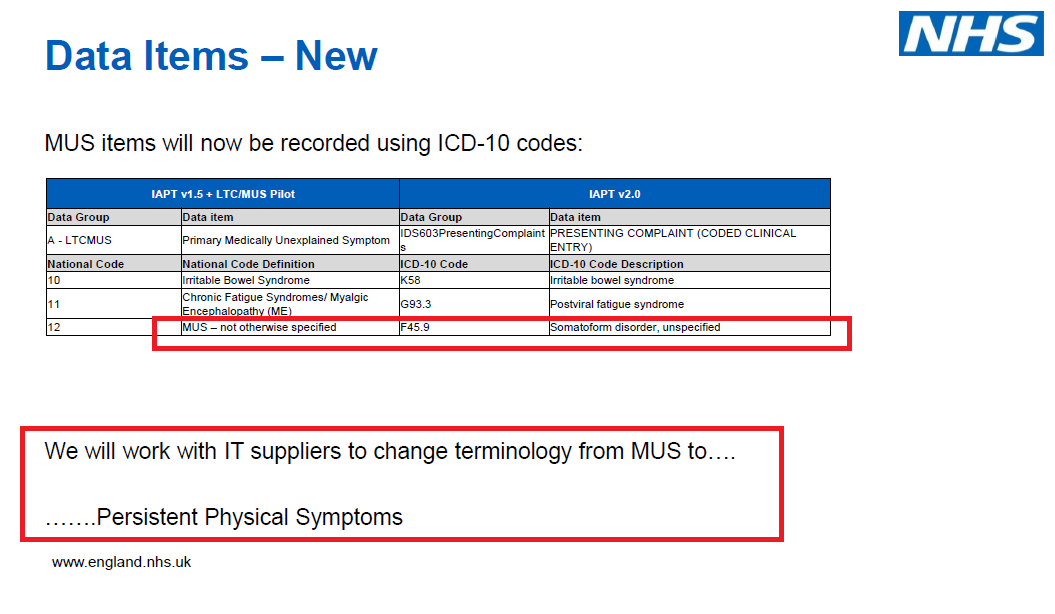
The American Psychiatric Association’s, 2013 DSM-5 abandoned the use of the term ‘medically unexplained symptoms’ for non-neurological disorders. In the UK, treatments for various medical illnesses with unexplained aetiology, such as chronic fatigue syndrome, irritable bowel syndrome and fibromyalgia, continue to fall under an MUS umbrella with cognitive behavioural therapy promoted as a primary therapeutic approach. In this editorial, we comment on whether the MUS concept is a viable diagnostic term, the credibility of the cognitive-behavioural MUS treatment model, the necessity of practitioner training and the validity of evidence of effectiveness in routine practice.
Open access, https://journals.sagepub.com/doi/10.1177/13591053211038042
The American Psychiatric Association’s, 2013 DSM-5 abandoned the use of the term ‘medically unexplained symptoms’ for non-neurological disorders. In the UK, treatments for various medical illnesses with unexplained aetiology, such as chronic fatigue syndrome, irritable bowel syndrome and fibromyalgia, continue to fall under an MUS umbrella with cognitive behavioural therapy promoted as a primary therapeutic approach. In this editorial, we comment on whether the MUS concept is a viable diagnostic term, the credibility of the cognitive-behavioural MUS treatment model, the necessity of practitioner training and the validity of evidence of effectiveness in routine practice.
Open access, https://journals.sagepub.com/doi/10.1177/13591053211038042