The Effects of a Mindfulness-Based Intervention on Depression and Anxiety in the Long-COVID Population
Long-COVID is a complicated, post-viral syndrome involving multiple body systems and can present with neuropsychiatric symptoms. Little has been reported about the neuropsychiatric symptoms of long-COVID, and validated treatments do not yet exist. There is prior evidence that mindfulness based strategies have been helpful for those with chronic illnesses; shown significant decreases in anxiety, stress, and depression; and enhanced quality of life. In this study, we report on the utility of a mindfulness-based intervention on levels of anxiety and depression in a long-COVID population.
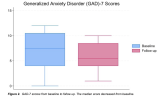
Our hospital system founded both a “Covid Recovery Clinic” (CRC) and a “Post-COVID Resilience Program” (PCRP). The PCRP consisted of a six-week virtual group therapy protocol that focused on mindfulness-based practices. Before and after the therapy intervention, participants answered questionnaires to capture depressive and anxiety symptoms.
Pre-and post-questionnaire scores do not show a significant improvement in depressive or anxiety symptoms, although the study was limited by a small sample size.
Further research is needed to investigate whether similar programs with a larger sample size can improve the mental health status of patients suffering from long-COVID.
Web | PDF | Journal of Patient-Centered Reviews and Research | Open Access
Rachel Welbel; Elizabeth Rutha; Jeffrey Ording; Douglas Wang; Jana Hirschtick
Long-COVID is a complicated, post-viral syndrome involving multiple body systems and can present with neuropsychiatric symptoms. Little has been reported about the neuropsychiatric symptoms of long-COVID, and validated treatments do not yet exist. There is prior evidence that mindfulness based strategies have been helpful for those with chronic illnesses; shown significant decreases in anxiety, stress, and depression; and enhanced quality of life. In this study, we report on the utility of a mindfulness-based intervention on levels of anxiety and depression in a long-COVID population.
Our hospital system founded both a “Covid Recovery Clinic” (CRC) and a “Post-COVID Resilience Program” (PCRP). The PCRP consisted of a six-week virtual group therapy protocol that focused on mindfulness-based practices. Before and after the therapy intervention, participants answered questionnaires to capture depressive and anxiety symptoms.
Pre-and post-questionnaire scores do not show a significant improvement in depressive or anxiety symptoms, although the study was limited by a small sample size.
Further research is needed to investigate whether similar programs with a larger sample size can improve the mental health status of patients suffering from long-COVID.
Web | PDF | Journal of Patient-Centered Reviews and Research | Open Access