Chandelier
Senior Member (Voting Rights)
Frontiers | Transcriptome analysis of classical blood cells reveals down-regulation of proinflammatory genes in the classical monocytes of Long-COVID patients
Despite extensive research, the pathogenesis and predispositions underlying Long-COVID remain poorly understood. To address this, we analyzed the immunologic...
Full title: Transcriptome analysis of classical blood cells reveals down-regulation of proinflammatory genes in the classical monocytes of Long-COVID patients
 Florian Fricke
Florian Fricke Franz Mai
Franz Mai


 Wendy Bergmann-Ewert
Wendy Bergmann-Ewert Marcel Kordt
Marcel Kordt Karin Kraft
Karin Kraft Britta Müller
Britta Müller Emil Christian Reisinger
Emil Christian Reisinger Brigitte Müller-Hilke*
Brigitte Müller-Hilke*Abstract
Despite extensive research, the pathogenesis and predispositions underlying Long-COVID remain poorly understood.
To address this, we analyzed the immunological landscapes of 44 Long-COVID patients and 44 matched convalescents using single-cell RNA sequencing (scRNA-seq) of peripheral blood mononuclear cells (PBMCs) and validated findings with plasma cytokine measurements via Luminex technology.
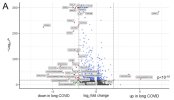
While immune cell compositions showed minimal quantitative differences only among NK cells, transcriptome analyses identified distinct gene expression patterns, particularly in classical monocytes: Long-COVID patients exhibited downregulation of inflammation-associated genes, including IL1B and CXCL2.
Imputation of transcription factor activity hinted at reduced inflammasome activity (via SNAI1) and impaired monocyte differentiation (via ATF2) in Long-COVID. RNA velocity supported the presence of immature classical monocytes in patients.
These findings showed that monocytes might be dysregulated and/or exhausted in Long-COVID patients.