Sly Saint
Senior Member (Voting Rights)
from Gabby Kleins blog:
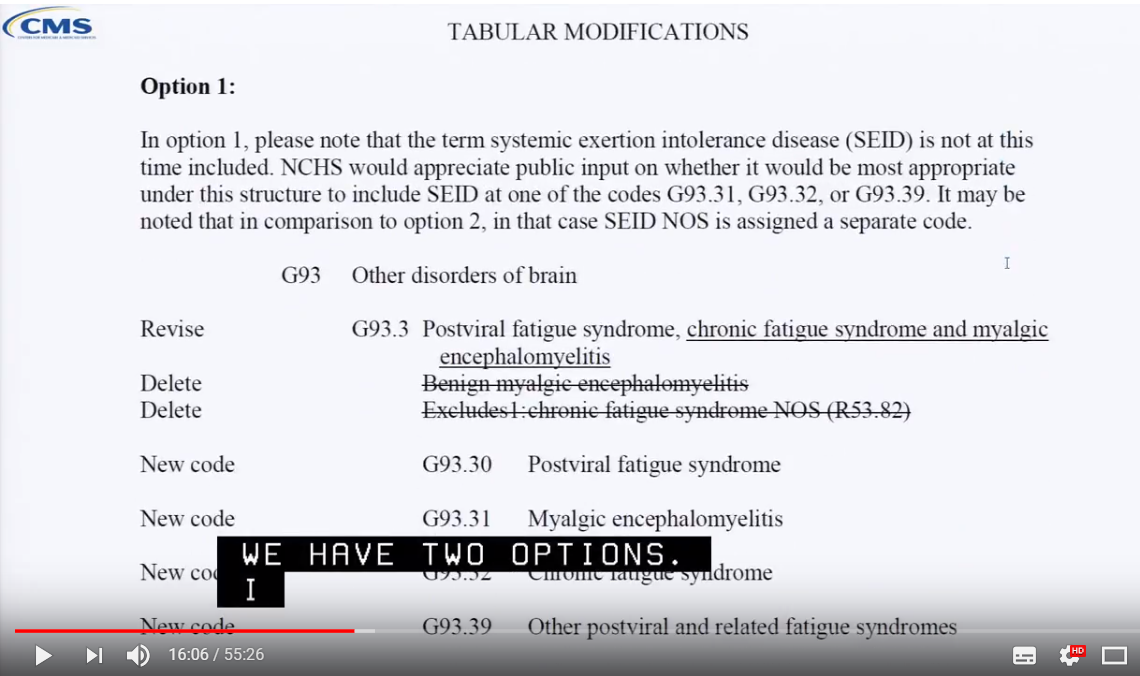
"A meeting took place on September 11 and 12, 2018 by the ICD-10 Coordination and Maintenance Committee.
On September 12, Donna Pickett discussed a proposal for “chronic fatigue syndrome”.
Dr. Lily Chu of the IACFS/ME called in with her approval of NCHS/CDC’s proposal for revised classifications for CFS and ME and a new classification for SEID."
"
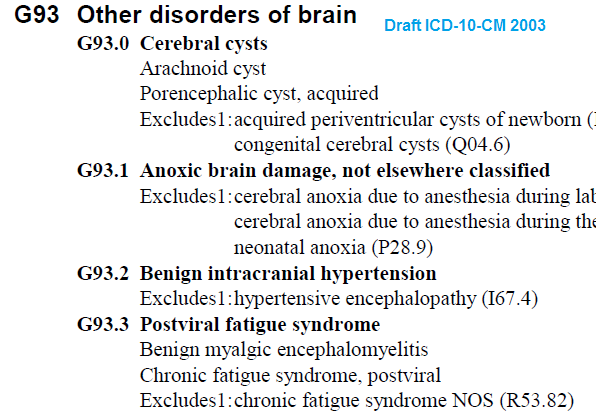
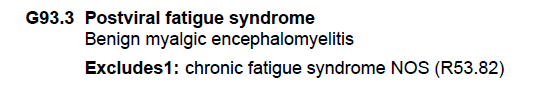
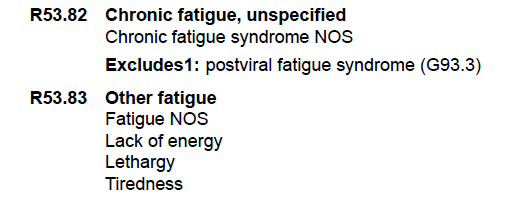
Proposed item changes under G93 – other disorders of the brain
there is a short video of the relevant bit of the meeting (I've not been able to watch it).
https://relatingtome.net/nchs-cdc-proposal-for-icd-10-cm/
eta: background info from Bateman Horne Center
https://batemanhornecenter.org/icd-10-code-for-mecfs/
"A meeting took place on September 11 and 12, 2018 by the ICD-10 Coordination and Maintenance Committee.
On September 12, Donna Pickett discussed a proposal for “chronic fatigue syndrome”.
Dr. Lily Chu of the IACFS/ME called in with her approval of NCHS/CDC’s proposal for revised classifications for CFS and ME and a new classification for SEID."
"
Proposed item changes under G93 – other disorders of the brain
- The title for G93.3 classification changed from Postviral to Postviral and other fatigue syndromes
- Benign Myalgic Encephalomyelitis changed to Myalgic Encephalomyelitis with new code – G93.32
- Switch chronic fatigue syndrome from R53.82 to new code – G93.33
- New item for systemic exertion intolerance disease with code G93.30
- New code for other postviral and related fatigue syndromes – G93.39"
there is a short video of the relevant bit of the meeting (I've not been able to watch it).
https://relatingtome.net/nchs-cdc-proposal-for-icd-10-cm/
eta: background info from Bateman Horne Center
https://batemanhornecenter.org/icd-10-code-for-mecfs/