Slide at
8:56 in video -
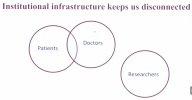
The Venn Diagram Result
View attachment 27207
How this relates to ME/CFS. Without an ME/CFS clinic to pool patients from, the researcher has no access to the doctors who look after these patients to get a full clinical picture, and it is so much harder to get patients for a study.
When they do get patients for a study, and see something different in a patient's data that might indicate a rare disease or needed medical follow up, their institution stops them from informing the patient, and they have no doctor to share that info with.
Yes I think that this is the one to focus on cracking for ME/CFS
'gatekeeping' has been a prime issue when you look at how it has been used particularly for anyone else to be able to do research into children and young people with ME/CFS and the sheer power that has provided certain clinics and researchers to tilt the literature by styming access (particularly when you add in that if they weren't stopping a project that they didn't like, then the FII insinuations is another worry for parents if they signed them up to a study someone 'overseeing their child' didn't approve of)
and I also mean that in a moving away from the fatigue and PPS bucketing sense.
I've said for years that in the absence of the correct type of other staff being available then it would be better to have good scientists with the right mindset running 'clinics'
than it would having motivational physios or OTs writing pretend pseudo-psych papers on the tiny part of the spectrum that they end up seeing from their bucket.
It would almost be interesting to draw up for our specific illness and different severities/stages what the hierarchy of usefulness/harmfulness of different types of staff would be if there really is some sort of shortage issue for whatever reason.
Of course I completely believe in the phrase
@rvallee has quoted a few times of whatever the system does is what it is supposed to do - if it wasn't working for those in charge they'd sure fix it, so I don't think the lack of diagnostics or triage has been an accident
and the nonsense move by certain individuals in clinical psychology to try and push 'transdiagnostic' just underlines that. Of course some people want to get away with selling things that don't ever cure people, but that they can sell indirectly (ie not to the patient or pupil but those who will decide for them) 'more is needed'.
I just can't tell why certain people who are supposed to be in charge of overseeing the health system for certain health systems want to sponsor that gravy train that just is a money-pit far more expensive and deskilling than the basic norm. Even for the short political cycle what gets proposed doesn't add up. And I don't think they are that stupid, and they can't all have been crooked or bad.
Is it just that they don't actually have the power to stop those who get to certain heavy-power positions at the top of the health service because of mechanisms that have been set up to theoretically protect somewhat backfiring?
At least finding a workaround so that absolute power isn't able to stymie all possible access routes to research or knowledge creation happenning would be a breakthrough. Although of course the questions of what mechanisms can stop trouble happening there are possible given the weaknesses we see in charities and who tends to rise to the top of different places crops up of course.
I think somewhere in this the answer is in codes of ethics/methods specific to ME/CFS type discussions that we have seen. There are projects that have been done very well like DecodeME and there should be something that can't be played but could serve as a useful checklist for patients to see whether a project is truly above board and protecting all the things like privacy/security and how data will be used, safety, accessibility, making sure there isn't protocol-switching half way through or funny inferences made on data etc.
 from the March event at UC Berkeley, where she unveils a bold vision for rare disease care .
from the March event at UC Berkeley, where she unveils a bold vision for rare disease care .