Activation of the Lectin Pathway Drives Persistent Complement Dysregulation in Long COVID
Long COVID affects a substantial proportion of survivors of acute infection with severe acute respiratory syndrome-associated coronavirus-2 (SARS-CoV-2), who suffer a variety of symptoms that limit their quality of life and economic activity. Although the aetiology of long COVID is obscure, it appears to be a chronic inflammatory condition. Complement dysregulation is a prevalent feature of long COVID. Specifically, markers of classical, alternative, and terminal pathway activation are often elevated in patients with this condition.
Here, we used a sensitive assay for mannan-binding lectin-associated serine protease-2 (MASP-2)/C1Inh complexes to analyse lectin pathway activation in a previously characterised cohort of patients with long COVID (n = 159) and healthy convalescent individuals with no persistent symptoms after infection with SARS-CoV-2 (n = 76). The data were combined with those from the most predictive complement analytes identified previously to delineate potential biomarkers of long COVID.
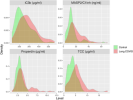
MASP-2/C1Inh complexes were significantly elevated in patients with long COVID (p = 0.0003). Generalised linear modelling further identified an optimal set of four markers, namely iC3b (alternative pathway), TCC (terminal pathway), MASP-2/C1Inh (lectin pathway), and the complement regulator properdin, which had a receiver operating characteristic predictive power of 0.796 (95% confidence interval = 0.664–0.905). Combinations of the classical pathway markers C4, C1q, and C1s/C1Inh were poorly predictive of long COVID.
These findings demonstrate that activation of the lectin complement pathway, which occurs upstream of the alternative and terminal pathways and can be inhibited therapeutically, is a salient feature of long COVID.
Web | DOI | PDF | Immunology | Open Access
Samuel B K Keat; Priyanka Khatri; Youssif M Ali; Chanuka H Arachchilage; Gregory Demopulos; Kirsten Baillie; Kelly L Miners; Kristin Ladell; Samantha A Jones; Helen E Davies; David A Price; Wioleta M Zelek; B Paul Morgan; Wilhelm J Schwaeble; Nicholas J Lynch
Long COVID affects a substantial proportion of survivors of acute infection with severe acute respiratory syndrome-associated coronavirus-2 (SARS-CoV-2), who suffer a variety of symptoms that limit their quality of life and economic activity. Although the aetiology of long COVID is obscure, it appears to be a chronic inflammatory condition. Complement dysregulation is a prevalent feature of long COVID. Specifically, markers of classical, alternative, and terminal pathway activation are often elevated in patients with this condition.
Here, we used a sensitive assay for mannan-binding lectin-associated serine protease-2 (MASP-2)/C1Inh complexes to analyse lectin pathway activation in a previously characterised cohort of patients with long COVID (n = 159) and healthy convalescent individuals with no persistent symptoms after infection with SARS-CoV-2 (n = 76). The data were combined with those from the most predictive complement analytes identified previously to delineate potential biomarkers of long COVID.
MASP-2/C1Inh complexes were significantly elevated in patients with long COVID (p = 0.0003). Generalised linear modelling further identified an optimal set of four markers, namely iC3b (alternative pathway), TCC (terminal pathway), MASP-2/C1Inh (lectin pathway), and the complement regulator properdin, which had a receiver operating characteristic predictive power of 0.796 (95% confidence interval = 0.664–0.905). Combinations of the classical pathway markers C4, C1q, and C1s/C1Inh were poorly predictive of long COVID.
These findings demonstrate that activation of the lectin complement pathway, which occurs upstream of the alternative and terminal pathways and can be inhibited therapeutically, is a salient feature of long COVID.
Web | DOI | PDF | Immunology | Open Access