Adrenergic dysfunction in patients with myalgic encephalomyelitis/chronic fatigue syndrome and fibromyalgia: A systematic review and meta-analysis
Jolien Hendrix; Lara Fanning; Arne Wyns; Ishtiaq Ahmed; Madhura Shekhar Patil; Emma Richter; Jente Van Campenhout; Kelly Ickmans; Rembert Mertens; Jo Nijs; Lode Godderis; Andrea Polli
BACKGROUND
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) are comorbid disorders with overlapping symptoms. Research highlights autonomic dysfunction compared to healthy individuals, particularly involving the sympathetic branch. While past reviews focused on neurophysiological assessments, this systematic review summarises biological adrenergic markers, offering deeper insights into the observed sympathetic dysfunction in ME/CFS and FM aiming to identify targetable pathophysiological mechanisms.
METHODS
A systematic search was performed on PubMed, Web of Science, Embase and Scopus. Studies investigating peripheral biological markers of adrenergic function in patients with ME/CFS or FM compared to healthy controls at baseline were included. Meta-analyses were performed using R statistical software.
RESULTS
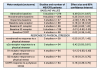
This meta-analysis of 37 studies, encompassing 543 ME/CFS patients and 651 FM patients, compared with 747 and 447 healthy controls, respectively, revealed elevated adrenaline (SMD = .49 [.31–.67]; Z = 5.29, p < .01) and β1 adrenergic receptor expression (SMD = .79 [.06–1.52]; Z = 2.13; p = .03) in blood of ME/CFS patients at rest. Additionally, patients with ME/CFS had a greater increase in the expression of α2A adrenergic receptor (AR, SMD = .57 [.18–.97]; Z = 2.85, p < .01), β2 AR (SMD = .41 [.02–.81]; Z = 2.04; p = .04) and COMT (SMD = .42 [.03–.81]; Z = 2.11; p = .03) after exercise and an increased response of noradrenaline to an orthostatic test (SMD = .11 [−.47 to −.70]; Z = 2.10; p = .04), both found in blood. FM patients showed no significant differences at baseline but exhibited a diminished adrenaline response to exercise (SMD = −.79 [−1.27 to −.30]; Z = −3.14; p < .01).
CONCLUSIONS
This systematic review and meta-analysis revealed adrenergic dysfunction mainly in patients with ME/CFS. Higher baseline adrenaline levels and atypical responses to exercise in ME/CFS indicate that sympathetic dysfunction, underscored by adrenergic abnormalities, is more involved in the pathophysiology of ME/CFS rather than FM.
Link | PDF (European Journal of Clinical Investigation)
Jolien Hendrix; Lara Fanning; Arne Wyns; Ishtiaq Ahmed; Madhura Shekhar Patil; Emma Richter; Jente Van Campenhout; Kelly Ickmans; Rembert Mertens; Jo Nijs; Lode Godderis; Andrea Polli
BACKGROUND
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) are comorbid disorders with overlapping symptoms. Research highlights autonomic dysfunction compared to healthy individuals, particularly involving the sympathetic branch. While past reviews focused on neurophysiological assessments, this systematic review summarises biological adrenergic markers, offering deeper insights into the observed sympathetic dysfunction in ME/CFS and FM aiming to identify targetable pathophysiological mechanisms.
METHODS
A systematic search was performed on PubMed, Web of Science, Embase and Scopus. Studies investigating peripheral biological markers of adrenergic function in patients with ME/CFS or FM compared to healthy controls at baseline were included. Meta-analyses were performed using R statistical software.
RESULTS
This meta-analysis of 37 studies, encompassing 543 ME/CFS patients and 651 FM patients, compared with 747 and 447 healthy controls, respectively, revealed elevated adrenaline (SMD = .49 [.31–.67]; Z = 5.29, p < .01) and β1 adrenergic receptor expression (SMD = .79 [.06–1.52]; Z = 2.13; p = .03) in blood of ME/CFS patients at rest. Additionally, patients with ME/CFS had a greater increase in the expression of α2A adrenergic receptor (AR, SMD = .57 [.18–.97]; Z = 2.85, p < .01), β2 AR (SMD = .41 [.02–.81]; Z = 2.04; p = .04) and COMT (SMD = .42 [.03–.81]; Z = 2.11; p = .03) after exercise and an increased response of noradrenaline to an orthostatic test (SMD = .11 [−.47 to −.70]; Z = 2.10; p = .04), both found in blood. FM patients showed no significant differences at baseline but exhibited a diminished adrenaline response to exercise (SMD = −.79 [−1.27 to −.30]; Z = −3.14; p < .01).
CONCLUSIONS
This systematic review and meta-analysis revealed adrenergic dysfunction mainly in patients with ME/CFS. Higher baseline adrenaline levels and atypical responses to exercise in ME/CFS indicate that sympathetic dysfunction, underscored by adrenergic abnormalities, is more involved in the pathophysiology of ME/CFS rather than FM.
Link | PDF (European Journal of Clinical Investigation)