Twitter summary here:
https://twitter.com/user/status/1831699391242989587
1) New blog post about catastrophizing and why this term risks blaming patients by mislabeling their symptoms as exaggerated negative thoughts.
2) Catastrophizing has been a popular topic because it is one of the most consistent psychological predictors of adverse pain outcomes. It is also central to the cognitive-behavioral model of ME/CFS.
There are, however, big problems with how the term has been implemented.
3) Catastrophizing was first introduced by Albert Ellis and later developed by Aaron Beck as a distorted thinking pattern in patients with mental and emotional problems. Their description focused on expecting the worst-case scenario in a situation that was far from catastrophic.
4) The problems arise when catastrophizing is used in patients with a severe, chronic disease. In such cases, it is difficult to differentiate between the severity of symptoms and catastrophizing thoughts.
A chronic illness itself is often a catastrophe that affects all aspects of life.
5) The most used tool to measure catastrophizing is the Pain Catastrophizing Scale (PCS). It does not focus on pessimistic forecasts of future events but on how people feel and think when they are experiencing pain.
6) It includes statements such as ‘It is awful and I feel that it overwhelms me’, ‘I keep thinking about how much it hurts’, or ‘I feel I cannot stand it anymore’ which might reflect the intensity of pain rather than how patients think about it.
7) Other items such as
‘There is nothing I can do to reduce the intensity of the pain’ might indicate how well a patient’s pain is being managed or how (un)successful treatments have been.
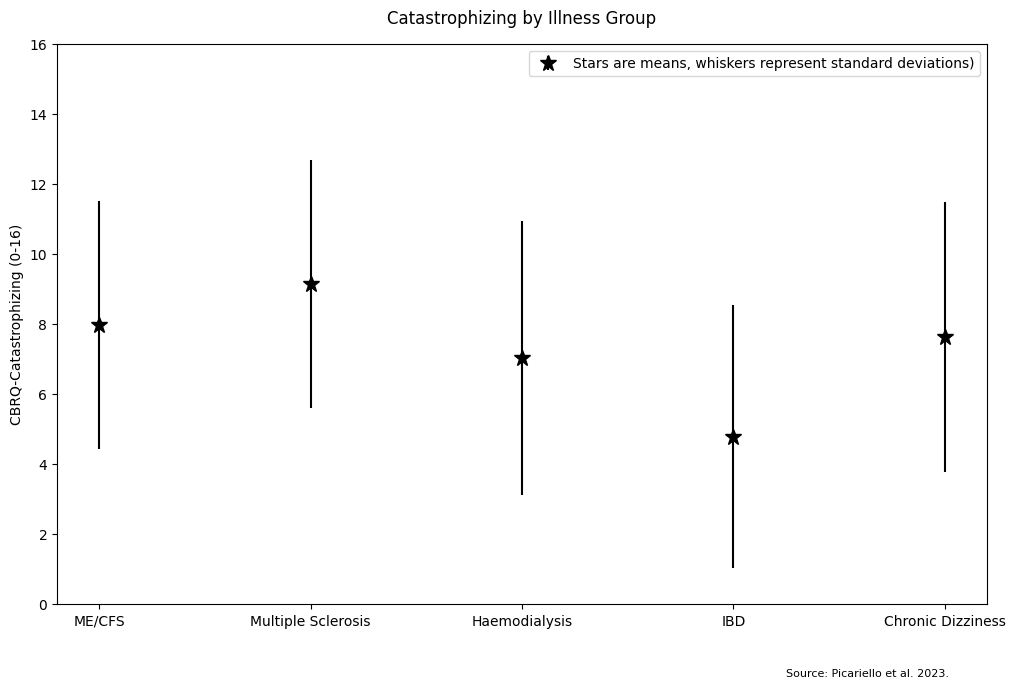
8) This mix-up could explain why the PCS correlates strongly with negative pain outcomes. It does not only measure an unhelpful thought pattern but also pain intensity, worry, distress, (unsuccessful) pain management, and other factors that patients know but the researchers likely don’t.
9) Unfortunately, patients and caregivers pay the price for these errors.
Patient surveys indicate that the term catastrophizing is blaming and demeaning and that healthcare professionals use it to deny pain medication or suggest that patients are exaggerating their symptoms.
10) Some proposed to rename the term to make it less stigmatizing but the underlying issue appears to run much deeper. What needs to change is the concept of catastrophizing itself.
11) One step forward is that some researchers have argued that pain catastrophizing cannot be assessed by self-report questionnaires because it requires contextual information and expert judgment.
12) Lastly, research on ME/CFS shows that patients do not have abnormally high catastrophizing scores when compared with other illnesses that have similar fatigue or illness duration.