I think one also has to admit that this wasn't only a BPS narrative but also a narrative spread by people believing in a "biological basis". For example Putrino and Iwasaki were giving widespread interviews on having found a "biological basis" and biomarkers for Long-Covid on the basis of results that anybody should be able to see couldn't stand the test of time.Would that disappoint those 1st responders who only want the stress-response option with a multiple choice MUS question to pass their easy-read neuro-rehab exam for re-enablement of crippled sufferers with medically unexplained, endearing but enduring and persistent symptoms of dysregulating, factitious, false illness-belief, which "we all believe and teach" making it the only realistic and pragmatic opportunity (by proxy)?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Arfmeister
Senior Member (Voting Rights)
We can almost close the thread I would have thought! Cortisol is clearly irrelevant.
I definitely wouldn’t close the thread. (But I know you’re not planning to do that
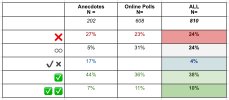
As I’m busy with analyzing the lowest quality data available : online polls and quantitive patient experiences - with glucocorticoids
- I still haven’t finalized this survey, but I already find it quite interesting
- therefore I’d like to give a snapshot of the data (but mind you it’s still work in progress and there’s a lot of detail I would like to lay out)
Reason I got interested in glucocorticoids is the remarkable improvement I got on a 4 week course of steroids (best improvement I ever had in 17 years). But always keep in mind, glucocorticoids are nasty drugs with a lot of long-term side effects.
Anyway, here is some preliminary data. When I have more conclusive data, I will post it with a lot more detail.
Overview ME-Patient experiences with:
- Hydrocortisone (cortisol equivalent)
- Prednisone / Prednisolone
- Methylprednisolone
- Dexamethasone
- Betamethasone
Last edited:
Thanks Arfmeister
e.g. this abstract from a 1988 study:
I believe that things like prednisone can induce feelings of wellbeing and high energy even in healthy people. So, I think that needs to be kept in mind when evaluating the impact of these drugs on people with ME/CFS. I'm actually surprised that there isn't a higher percentage of people reporting a benefit.It’s not based on supposedly low cortisol in ME/LC - but on a big ME-subgroup that had benefits from supplementing in cortisol
e.g. this abstract from a 1988 study:
It is a clinical impression that some patients given oral corticosteroids develop a sense of wellbeing that is 'inappropriate' to improvements in physical health. This has been termed steroid 'euphoria', but unlike steroid-induced psychosis it has not been documented. To test for the size and frequency of this phenomenon, 20 patients with severe chronic obstructive airways disease (mean FEV1 0.86 l) were given 30 mg of prednisolone for 14 days, after a period of placebo administration in a single-blind study.
Lung spirometry and arterial saturation during exercise were measured serially, together with established measures of mood state. No changes in spirometry or arterial saturation during exercise were detected until 7 days of active therapy. Mood state did not change during the placebo period, but small significant reductions in anxiety and depression were measured after 3 days of prednisolone and before any measurable improvement in lung function. Mood state did not then further improve, despite measurable improvements in lung spirometry.
This is evidence that prednisolone may produce a mild 'inappropriate' sense of wellbeing within a population receiving the drug, rather than as an occasional idiosyncratic response.
Lou B Lou
Senior Member (Voting Rights)
Thanks Arfmeister
I believe that things like prednisone can induce feelings of wellbeing and high energy even in healthy people. So, I think that needs to be kept in mind when evaluating the impact of these drugs on people with ME/CFS. I'm actually surprised that there isn't a higher percentage of people reporting a benefit.
e.g. this abstract from a 1988 study:
@Hutan wrote - "I believe that things like prednisone can induce feelings of wellbeing and high energy even in healthy people."
I had a course of high dose Prednisolone from early September. 40mgs for 4 weeks then gradually reduction (still reducing very slowly).
I definitely had the feelings of wellbeing on the higher dose, down to 25mgs, but definitely no increase in energy.
I had my normal ME response to the additional appointments, which was PEM (GP and hospital, travelling, upright in waiting rooms, walking around the hospital, medical investigations that led to the prescribing of prednisolone, the prescribing was nothing to do with ME).
The feelings of wellbeing were not really euphoria, but were quite pleasant and meant I was not as fed up as I probably should have been.
Last edited:
Jonathan Edwards
Senior Member (Voting Rights)
Yes, there are various reasons why one would expect steroids to help people feel better, at least short term, but it is crucial to note that this has no bearing on the question as to whether abnormal steroid regulation contributes to ME/CFS symptoms. That link would be non-sequitur.
Arfmeister
Senior Member (Voting Rights)
Yes. There’s many patients that had positive effects during steroids, but the negative side effects coming off steroids classified it as negative or even keel. Steroids hangover.I'm actually surprised that there isn't a higher percentage of people reporting a benefit.
- "I believe that things like prednisone can induce feelings of wellbeing and high energy even in healthy people."
But does euphoria account for:
- increase PEM threshold (from bed/housebound to being temporary very mild)
- lower orthostatic intolerance from first day(s)
- Erase brain fog (e.g bringing old forgotten memories back)
- Or in some cases complete temporary remission
*this is some examples from various good responders
@Hutan What is your experience with steroids, if I may ask?
Last edited by a moderator:
Lou B Lou
Senior Member (Voting Rights)
Yes. There’s many patients that had positive effects during steroids, but the negative side effects coming off steroids classified it as negative or even keel. Steroids hangover.
But does euphoria account for:
All for the time taking (higher than replacement dosage) steroids* ?
- increase PEM threshold (from bed/housebound to being temporary very mild)
- lower orthostatic intolerance from first day(s)
- Erase brain fog (e.g bringing old forgotten memories back)
- Or in some cases complete temporary remission
*this is some examples from various good responders
@Hutan What is your experience with steroids, if I may ask?
The reason I was prescribed prednisolone (and high dose cortisone body cream) had nothing to do with ME, but was for a very recent auto immune disease called Bullous Pemphigoid.
By feelings of wellbeing I mean I felt quite good in my head on the higher doses. But there was no corresponding improvement in the state of my body health or any ME symptoms.
I had no improvement in ME, no improved energy, no increase in PEM threshold, no improved cognitive function, no improvement in OI.
I was (and remain) more ill in ME terms while taking prednisolone, with PEM, needing to be in bed more not less. And still am (am still reducing the medication dose).
I first put that down to having had to attend GP and hospital appointments in September, with travelling, and hours at the hospital having tests and biopsy. Then a week and a half of daily phone calls chasing up my prescriptions as there was a difference of (NHS) opinion as to who was supposed to be doing the prescribing, and the pharmacy got confused between all the various prescriptions. That caused a gap of days with no medication and I had to start the course of prednisolone again. Then there was an arduous daily regime of applying cortisone cream for months.
I'm still more sick in ME terms now than before I started the prednisolone in early September. I don't know if it's the additional disease that's taking it out of me, or the medication, or what.
Edit add
I did notice after reducing the prednisolone (Very Gradually, Incrementally) to about 25/20 mgs a day, that I was having 2/3/4 days of low mood after each incremental reduction in dose. I don't normally suffer with low mood. I worked out it was just the medication reduction and just put up with it until around 4 days after reduction my mood just evened out and I felt fine again.
I do think that Drs should warn patients about that effect from the necessary reduction of prednisolone dosage. As I said, I don't suffer with low mood normally, I worked out it was just the medication reduction, and was able to just ride it out until my mood seemed to even out and I felt fine again. BUT, for patients who do suffer with low mood before taking the medication, the prednisolone reduction effects could be more serious or disturbing.
.
Last edited:
On hydrocortisone treatment, this is a copy of a post I made on another thread:
There were 70 people with CFS assessed in this 1998 study. Average baseline morning cortisol, and cortisol after stimulation with ACTH were completely normal. Positive responses to hydrocortisone treatment were limited to one questionnaire among quite a number, were small and were in line with the positive response that healthy people also experience. The authors (including Wessely) themselves concluded that hydrocortisone treatment caused substantially more harm than benefit, sayingThought I'd create a thread for the referenced paper on hydrocortisone treatment in CFS, Low-Dose Hydrocortisone for Treatment of Chronic Fatigue Syndrome - A Randomized Controlled Trial, 1998, McKenzie et al
We found that low-dose hydrocortisone treatment has mild side effects (Table 3) and affords minimal therapeutic benefit for CFS
I can't recall having steroids since developing ME/CFS.@Hutan What is your experience with steroids, if I may ask?
Possible Involvement of Hypothalamic Dysfunction in Long COVID Patients Characterized by Delayed Response to Gonadotropin-Releasing Hormone (2026)
Table 2. Basal hormone levels of long COVID patients who underwent pituitary stimulation tests.
Cortisol (µg/dL)
7.5 ± 0.8 (Reference range: 7.1–19.6)
in the present patients with long COVID, the peak ACTH and cortisol responses to CRH and their recovery levels at 120 min were nearly normal, failing to detect clear HPA axis abnormalities. Furthermore, assessment of basal cortisol secretion using 24 h urinary collection (UFC) revealed a nearly normal level of approximately 40 µg/day.
Arfmeister
Senior Member (Voting Rights)
I have been reading some of the S4ME threads on cortisol (a lot !) including the patient trials and I was wondering the following:Average baseline morning cortisol, and cortisol after stimulation with ACTH were completely normal.
In many studies, it appears that in ME cortisol levels are (close to) normal. Although morning cortisol is lower vs healthy controls and overall cortisol levels seems more flattened / blunted over the day.
My thinking : cortisol levels are normal or low for most ME patients. Never or seldom high levels.
In PEM, ME patients are not able to handle any form of physical or neurological stress in a proper way
So is it possible that part of the problem is: that when ME-patients get in a PEM crash they fail to mount a proper cortisol response - so they fail to dampen the crash ?
- So for some reason the HPA axis is not able to increase cortisol during PEM ⇒ therefore (neuro)inflammation is not managed properly
- The cortisol production is blunted, and insufficient to shut down the inflammation and increased stress on the body
- This could be part of the reason that exertional triggers and (small) immune triggers (like bacteria,virus) produce outsized + prolonged crashes (as the lack of increase cortisol can not help in extinguishing the fire)
Ergo, the HPA-axis functions properly with no problems ACTH / Cortisol production.
- But maybe CRH input or production is too low?
- Because a default neuro-immune signaling that triggers sickness behavior ?
- Which causes a failure to stimulate the HPA axis - specifically during long periods of exertion ?
- As specifically endurance type exercise normally creates high level of cortisol ?
Have you ever come across any research publication that measured cortisol and ACTH levels during PEM ?
- Would be interesting to know if cortisol was measured during PEM crash - e.g. after exertion, ideally a 2-day CPET test
This has my interest because of my own experience :
- My morning cortisol and ACTH were measured before breakfast in serum in a moderate PEM state - on 2 different occasions. Values were both at the (very) low end, but just within range.
- During PEM, my body nor my psyche can handle stress well. My body aches, strong headache and brain fog - with neural inflammation/microglia as culprits IMO.
- As an example of inflammation during PEM: I have my seboric dermatitis flare up during PEM as ‘proof’ that inflammation is increased
- Additionally,I have been improved a lot on a 1 month high dosage steroids protocol: it increased my PEM threshold immensely - from 1 step/day to 300 sustainable steps - and system wide ME-improvement
- which to me can impossibly be ascribed to euphoria (OR if so: dopamine is one of the core issues with (my) ME - or placebo can come unexpected )
Last edited:
Measurements before and 1 day after CPET/exercise might provide an approximation to PEM. There have been some studies that have measured molecules in the blood before and after exercise. I can't recall one that measured cortisol but possibly some have.Have you ever come across any research publication that measured cortisol and ACTH levels during PEM ?
Another sort of study would be 'good day, bad day' studies with molecule measurements, with 'bad days' presumably being more likely to be PEM days. @MelbME has been doing some studies like that I think, including one in a pediatric cohort.
There have been a lot of studies measuring cortisol in people with ME/CFS, and generally, as this thread demonstrates, no difference is found. If PEM was significantly depressing cortisol levels, I think we'd see a pattern of a substantial percentage of participants having low cortisol, and we don't routinely see that.
Studies of cortisol levels in people with (very)severe ME/CFS could be useful in answering the question of what happens to cortisol during PEM, as I think they might be in PEM most of the time. But, I'm sure we'd know by now if people with severe ME/CFS really had abnormally low cortisol.
My experience high morning cortisol but after 3 yrs zopiclone and probably a rebound, cold turkey phenomenon, which for some strange reason was worsened by MgEAP (very strange but I think the case) But low cortisol after heavy (spoonful) nystatin dose. I think Teitelbaum mentions low cortisol in association with candida and die off. Not tested for yrs now. Low cortisol often occurs in sarcoid but usually put down to prednisolone use. Pred itself makes me dopy and I have hardly used it. Endogenous cortisol sometimes high in sarcoid (hair) as body possibly tries to suppress inflammation. Don't know if this might promote adrenal fatigue (as might the "work" of dragging yourself around all the time). Parallels with ME might be drawn by those who claim ME as inflammatory - if there is a single ME.
Shared autonomic phenotype of long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (2026)
We were unable to detect hormonal changes indicative of adrenal or hypothalamic-pituitary-adrenal axis insufficiency, as evidenced by normal cortisol and ACTH levels across our studied groups.
patient’s charts were reviewed for laboratory blood evaluations conducted during routine clinical assessments.
Normal range: 6.0–18.4 µg/dL
ME/CFS (n=170): 10.60 (5.23)
LC (n=143): 11.15 (6.58)
hEDS (n=290): 13.55 (6.70)
Arfmeister
Senior Member (Voting Rights)
This was taken in the morning, presumably?
Anyway, Whatever the time of day, it confirms previous findings - and remarks in this thread:
- ME CFS cortisol is (somewhat) lower than healthy people
- I presume there were no healthy controls in the study?
Note: For a healthy adult with a regular sleep schedule, the average morning cortisol level is:
• 15 µg/dL (US)
• 414 nmol/L (EU)
I'm very severe in the dark all the time so if anything my cortisol should be messed up but to the contrary, if I manage to schedule the blood test after waking and not super late/early my cortisol is pretty much average to slighly above average. I also have a very consistent sleep schedule. I also did several 4 point salivary cortisol tests and all have been normal.
Could the abnormal findings here be correlated with bad/reversed sleep schedules or bad timing of taking the blood?
Could the abnormal findings here be correlated with bad/reversed sleep schedules or bad timing of taking the blood?
A small 2001 study
Abnormalities in response to vasopressin infusion in chronic fatigue syndrome
Abnormalities in response to vasopressin infusion in chronic fatigue syndrome
Not significantly different.Mean basal cortisol level was 9.2±0.4 ug/dl in the patients and 8.0±0.5 ug/dl in the control group.
There's a discussion of cortisol levels in cerebrospinal fluid on this thread
Loss of CRH neurons and other neural changes in ME/CFS autopsy study, University of Amsterdam
The discussion covers the results from the NIH Walitt et al Deep Phenotyping study, with the cerebrospinal fluid levels plotted in a chart by @forestglip at post #129 showing no differences between the ME/CFS and control groups.
This contrasts with the results reported for the autopsy study (although not published yet), where the average cerebrospinal cortisol for the people with ME/CFS (shown in red) was almost zero.

There is discussion about how that finding from the autopsy study could have come about, but, given the study has not been published yet, it is speculative.
Loss of CRH neurons and other neural changes in ME/CFS autopsy study, University of Amsterdam
The discussion covers the results from the NIH Walitt et al Deep Phenotyping study, with the cerebrospinal fluid levels plotted in a chart by @forestglip at post #129 showing no differences between the ME/CFS and control groups.
This contrasts with the results reported for the autopsy study (although not published yet), where the average cerebrospinal cortisol for the people with ME/CFS (shown in red) was almost zero.

There is discussion about how that finding from the autopsy study could have come about, but, given the study has not been published yet, it is speculative.
Last edited:
Jonathan Edwards
Senior Member (Voting Rights)
This contrasts with the results reported for the autopsy study (although not published yet), where the average cerebrospinal cortisol for the people with ME/CFS (shown in red) was almost zero.
Did you mean that? I thought these data were CRH cells in brain rather than cortisol?
Jonathan Edwards
Senior Member (Voting Rights)
Fixed. Overall effect is pretty similar.
Ah. I had not seen that. I think I now understand your previous comment about the low levels being related by some common artifactual influence. The apparent absence of cortisol in CSF makes no real sense as consequence of depleted CRH cells unless these cases are unusual instances of pre-terminal adrenal failure it seems. I think we need to see detailed published findings.
