Evidence of Accumulating Neurophysiologic Dysfunction in Persistent Post-COVID Fatigue
[Line breaks added]
Abstract
A major consequence of the COVID-19 pandemic has been the emergence of post-COVID syndrome (PCS), and more specifically, post-COVID fatigue (pCF), with an estimated prevalence of ~2%. We previously showed that, compared to healthy controls, people with pCF exhibit changes in muscle physiology, cortical circuitry, and autonomic function.
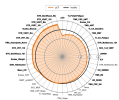
Here we present results from a cohort of people with pCF (N=145), between 12 weeks and 45 months post-infection. We report self-perception of fatigue; objective measures of cortical circuits via transcranial magnetic stimulation and reaction time tasks; peripheral muscle fatigue; and autonomic function such as heart rate variability.
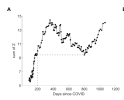
Those with pCF persisting >200 days had significantly more fatigue and showed increased cortical excitability, slower reaction times and increased peripheral muscle fatigue compared to those with <200 days of pCF .
In pCF, if there is no spontaneous recovery, fatigue worsens, and patients continue to accumulate significant neurophysiologic abnormalities.
Web | PDF | DOI | medRxiv | Preprint
Germann, Maria; Maffitt, Natalie J; Burton, Olivia A; Ashhad, Amn; Baker, Anne M.E.; Zaaimi, Boubker; Ng, Wan-Fai; Soteropoulos, Demetris S; Baker, Stuart N; Baker, Mark R
[Line breaks added]
Abstract
A major consequence of the COVID-19 pandemic has been the emergence of post-COVID syndrome (PCS), and more specifically, post-COVID fatigue (pCF), with an estimated prevalence of ~2%. We previously showed that, compared to healthy controls, people with pCF exhibit changes in muscle physiology, cortical circuitry, and autonomic function.
Here we present results from a cohort of people with pCF (N=145), between 12 weeks and 45 months post-infection. We report self-perception of fatigue; objective measures of cortical circuits via transcranial magnetic stimulation and reaction time tasks; peripheral muscle fatigue; and autonomic function such as heart rate variability.
Those with pCF persisting >200 days had significantly more fatigue and showed increased cortical excitability, slower reaction times and increased peripheral muscle fatigue compared to those with <200 days of pCF .
In pCF, if there is no spontaneous recovery, fatigue worsens, and patients continue to accumulate significant neurophysiologic abnormalities.
Web | PDF | DOI | medRxiv | Preprint