Familial coaggregation and shared familiality of functional and internalizing disorders in the Lifelines cohort
Martje Bos, Rei Monden, Naomi R. Wray, Yiling Zhou, Kenneth S. Kendler, Judith G. M. Rosmalen, Hanna M. van Loo, Harold Snieder
[Line breaks added]
Background
Functional disorders (FDs) are characterized by persistent somatic symptoms and are highly comorbid with internalizing disorders (IDs). To provide much-needed insight into FD etiology, we evaluated FD and ID familial coaggregation and shared familiality.
Methods
Lifelines is a three-generation cohort study, which assessed three FDs (myalgic encephalomyelitis/chronic fatigue syndrome [ME/CFS], irritable bowel syndrome [IBS], and fibromyalgia [FM]) and six IDs (major depressive disorder [MDD], dysthymia [DYS], generalized anxiety disorder [GAD], agoraphobia [AGPH], social phobia [SPH], and panic disorder [PD]) according to diagnostic criteria.
Based on 153,803 individuals, including 90,397 with a first-degree relative in Lifelines, we calculated recurrence risk ratios (λRs) and tetrachoric correlations to evaluate familial aggregation and coaggregation of these disorders in first-degree relatives. We then estimated their familiality and familial correlations.
Results
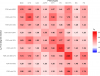
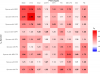
Familial aggregation was observed across disorders, with λR ranging from 1.45 to 2.23 within disorders and from 1.17 to 1.94 across disorders.
Familiality estimates ranged from 22% (95% confidence interval [CI]: 16–29) for IBS to 42% (95% CI: 33–50) for ME/CFS.
Familial correlations ranged from +0.37 (95% CI: 0.24–0.51) between FM and AGPH to +0.97 (95% CI: 0.80–1) between ME/CFS and FM.
The highest familial correlation between an ID and FD was +0.83 (95% CI: 0.66–0.99) for MDD and ME/CFS.
Conclusions
There is a clear familial component to FDs, which is partially shared with IDs. This suggests that IDs and FDs share both genetic and family-environmental risk factors. Of the FDs, ME/CFS is most closely related to IDs.
Link | PDF (Psychological Medicine) [Open Access]
Martje Bos, Rei Monden, Naomi R. Wray, Yiling Zhou, Kenneth S. Kendler, Judith G. M. Rosmalen, Hanna M. van Loo, Harold Snieder
[Line breaks added]
Background
Functional disorders (FDs) are characterized by persistent somatic symptoms and are highly comorbid with internalizing disorders (IDs). To provide much-needed insight into FD etiology, we evaluated FD and ID familial coaggregation and shared familiality.
Methods
Lifelines is a three-generation cohort study, which assessed three FDs (myalgic encephalomyelitis/chronic fatigue syndrome [ME/CFS], irritable bowel syndrome [IBS], and fibromyalgia [FM]) and six IDs (major depressive disorder [MDD], dysthymia [DYS], generalized anxiety disorder [GAD], agoraphobia [AGPH], social phobia [SPH], and panic disorder [PD]) according to diagnostic criteria.
Based on 153,803 individuals, including 90,397 with a first-degree relative in Lifelines, we calculated recurrence risk ratios (λRs) and tetrachoric correlations to evaluate familial aggregation and coaggregation of these disorders in first-degree relatives. We then estimated their familiality and familial correlations.
Results
Familial aggregation was observed across disorders, with λR ranging from 1.45 to 2.23 within disorders and from 1.17 to 1.94 across disorders.
Familiality estimates ranged from 22% (95% confidence interval [CI]: 16–29) for IBS to 42% (95% CI: 33–50) for ME/CFS.
Familial correlations ranged from +0.37 (95% CI: 0.24–0.51) between FM and AGPH to +0.97 (95% CI: 0.80–1) between ME/CFS and FM.
The highest familial correlation between an ID and FD was +0.83 (95% CI: 0.66–0.99) for MDD and ME/CFS.
Conclusions
There is a clear familial component to FDs, which is partially shared with IDs. This suggests that IDs and FDs share both genetic and family-environmental risk factors. Of the FDs, ME/CFS is most closely related to IDs.
Link | PDF (Psychological Medicine) [Open Access]