Data-independent LC-MS/MS analysis of ME/CFS plasma reveals a dysregulated coagulation system, endothelial dysfunction, downregulation of complement machinery
Massimo Nunes, Mare Vlok, Amy Proal, Douglas B. Kell, Etheresia Pretorius
Published 16 July 2024
Abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating chronic condition that is characterized by unresolved fatigue, post-exertion symptom exacerbation (PESE), cognitive dysfunction, orthostatic intolerance, and other symptoms. ME/CFS lacks established clinical biomarkers and requires further elucidation of disease mechanisms. A growing number of studies demonstrate signs of hematological and cardiovascular pathology in ME/CFS cohorts, including hyperactivated platelets, endothelial dysfunction, vascular dysregulation, and anomalous clotting processes.
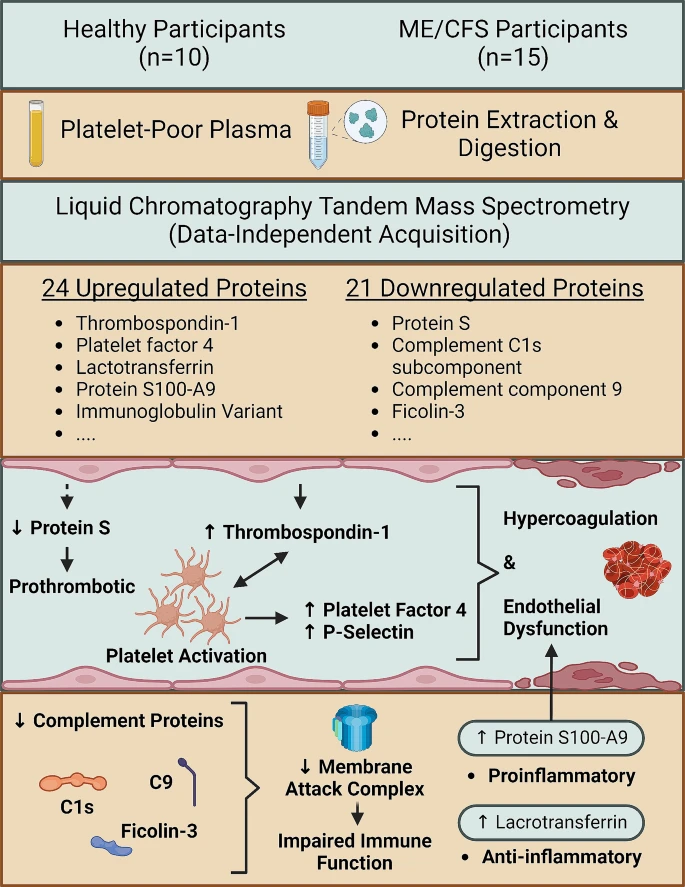
To build on these findings, and to identify potential biomarkers that can be related to pathophysiology, we measured differences in protein expression in platelet-poor plasma (PPP) samples from 15 ME/CFS study participants and 10 controls not previously infected with SARS-CoV-2, using DIA LC-MS/MS.
We identified 24 proteins that are significantly increased in the ME/CFS group compared to the controls, and 21 proteins that are significantly downregulated. Proteins related to clotting processes – thrombospondin-1 (important in platelet activation), platelet factor 4, and protein S – were differentially expressed in the ME/CFS group, suggestive of a dysregulated coagulation system and abnormal endothelial function. Complement machinery was also significantly downregulated, including C9 which forms part of the membrane attack complex. Additionally, we identified a significant upregulation of lactotransferrin, protein S100-A9, and an immunoglobulin variant.
The findings from this experiment further implicate the coagulation and immune system in ME/CFS, and bring to attention the pathology of or imposed on the endothelium. This study highlights potential systems and proteins that require further research with regards to their contribution to the pathogenesis of ME/CFS, symptom manifestation, and biomarker potential, and also gives insight into the hematological and cardiovascular risk for ME/CFS individuals affected by diabetes mellitus.
Graphical abstract
Link (Cardiovascular Diabetology) [Open access]
Massimo Nunes, Mare Vlok, Amy Proal, Douglas B. Kell, Etheresia Pretorius
Published 16 July 2024
Abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating chronic condition that is characterized by unresolved fatigue, post-exertion symptom exacerbation (PESE), cognitive dysfunction, orthostatic intolerance, and other symptoms. ME/CFS lacks established clinical biomarkers and requires further elucidation of disease mechanisms. A growing number of studies demonstrate signs of hematological and cardiovascular pathology in ME/CFS cohorts, including hyperactivated platelets, endothelial dysfunction, vascular dysregulation, and anomalous clotting processes.
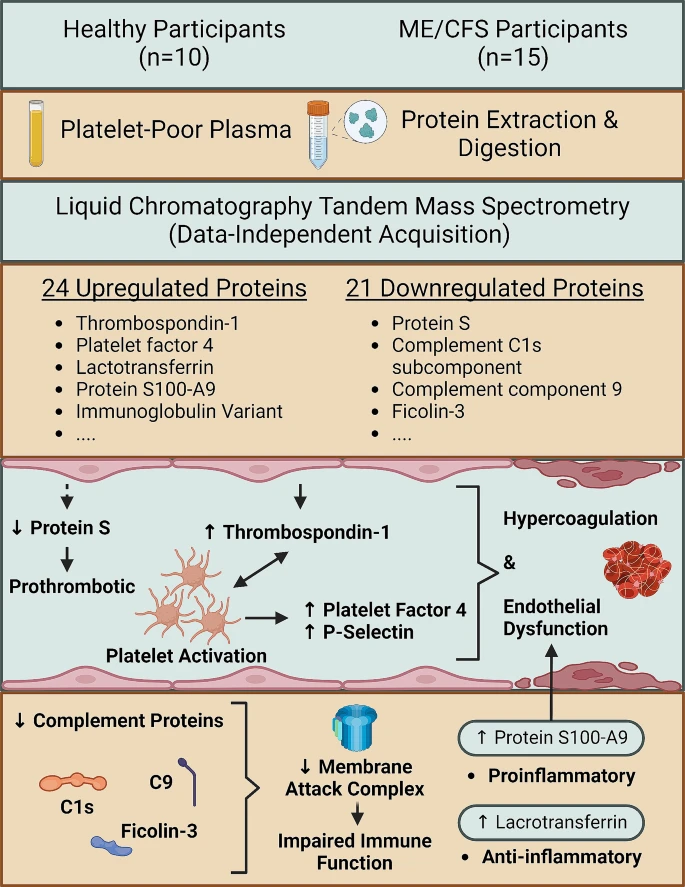
To build on these findings, and to identify potential biomarkers that can be related to pathophysiology, we measured differences in protein expression in platelet-poor plasma (PPP) samples from 15 ME/CFS study participants and 10 controls not previously infected with SARS-CoV-2, using DIA LC-MS/MS.
We identified 24 proteins that are significantly increased in the ME/CFS group compared to the controls, and 21 proteins that are significantly downregulated. Proteins related to clotting processes – thrombospondin-1 (important in platelet activation), platelet factor 4, and protein S – were differentially expressed in the ME/CFS group, suggestive of a dysregulated coagulation system and abnormal endothelial function. Complement machinery was also significantly downregulated, including C9 which forms part of the membrane attack complex. Additionally, we identified a significant upregulation of lactotransferrin, protein S100-A9, and an immunoglobulin variant.
The findings from this experiment further implicate the coagulation and immune system in ME/CFS, and bring to attention the pathology of or imposed on the endothelium. This study highlights potential systems and proteins that require further research with regards to their contribution to the pathogenesis of ME/CFS, symptom manifestation, and biomarker potential, and also gives insight into the hematological and cardiovascular risk for ME/CFS individuals affected by diabetes mellitus.
Graphical abstract
Link (Cardiovascular Diabetology) [Open access]
Last edited:

