https://pubmed.ncbi.nlm.nih.gov/9989716/
A J Cleare 1, E Heap, G S Malhi, S Wessely, V O'Keane, J Miell
Abstract
Background: Reports of mild hypocortisolism in chronic fatigue syndrome led us to postulate that low-dose hydrocortisone therapy may be an effective treatment.
Methods: In a randomised crossover trial, we screened 218 patients with chronic fatigue. 32 patients met our strict criteria for chronic fatigue syndrome without co-morbid psychiatric disorder. The eligible patients received consecutive treatment with low-dose hydrocortisone (5 mg or 10 mg daily) for 1 month and placebo for 1 month; the order of treatment was randomly assigned. Analysis was by intention to treat.
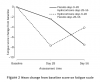
Findings: None of the patients dropped out. Compared with the baseline self-reported fatigue scores (mean 25.1 points), the score fell by 7.2 points for patients on hydrocortisone and by 3.3 points for those on placebo (paired difference in mean scores 4.5 points [95% CI 1.2-7.7], p=0.009). In nine (28%) of the 32 patients on hydrocortisone, fatigue scores reached a predefined cut-off value similar to the normal population score, compared with three (9%) of the 32 on placebo (Fisher's exact test p=0.05). The degree of disability was reduced with hydrocortisone treatment, but not with placebo. Insulin stress tests showed that endogenous adrenal function was not suppressed by hydrocortisone. Minor side-effects were reported by three patients after hydrocortisone treatment and by one patient after placebo.
Interpretation: In some patients with chronic fatigue syndrome, low-dose hydrocortisone reduces fatigue levels in the short term. Treatment for a longer time and follow-up studies are needed to find out whether this effect could be clinically useful.
A J Cleare 1, E Heap, G S Malhi, S Wessely, V O'Keane, J Miell
Abstract
Background: Reports of mild hypocortisolism in chronic fatigue syndrome led us to postulate that low-dose hydrocortisone therapy may be an effective treatment.
Methods: In a randomised crossover trial, we screened 218 patients with chronic fatigue. 32 patients met our strict criteria for chronic fatigue syndrome without co-morbid psychiatric disorder. The eligible patients received consecutive treatment with low-dose hydrocortisone (5 mg or 10 mg daily) for 1 month and placebo for 1 month; the order of treatment was randomly assigned. Analysis was by intention to treat.
Findings: None of the patients dropped out. Compared with the baseline self-reported fatigue scores (mean 25.1 points), the score fell by 7.2 points for patients on hydrocortisone and by 3.3 points for those on placebo (paired difference in mean scores 4.5 points [95% CI 1.2-7.7], p=0.009). In nine (28%) of the 32 patients on hydrocortisone, fatigue scores reached a predefined cut-off value similar to the normal population score, compared with three (9%) of the 32 on placebo (Fisher's exact test p=0.05). The degree of disability was reduced with hydrocortisone treatment, but not with placebo. Insulin stress tests showed that endogenous adrenal function was not suppressed by hydrocortisone. Minor side-effects were reported by three patients after hydrocortisone treatment and by one patient after placebo.
Interpretation: In some patients with chronic fatigue syndrome, low-dose hydrocortisone reduces fatigue levels in the short term. Treatment for a longer time and follow-up studies are needed to find out whether this effect could be clinically useful.