mariovitali
Senior Member (Voting Rights)
First of all, Thank you for the reply. Much appreciated.Thanks. If I understand correctly, though, your network analysis is based on mentions in abstracts and the text of a publication and not on the actual data of studies?
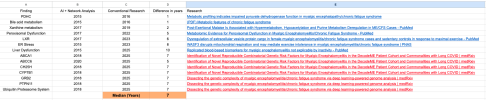
What you say is correct. All of the work that was made was an attempt to connect medical concepts that have been appearing to the text of the abstracts. This was the first part of the work , the Network Analysis (which was later used by Wenzhong Xiao).
The second part of the work was taking the various symptoms of MECFS, retrieving abstracts related to each of these symptoms and then asking from machine learning to tell us which combination of topics could predict a symptom vs a non-symptom state.
I do not quite understand what you mean with "actual data" of studies so I would appreciate your time in explaining what this means. But for the moment let's look at results so far given the input I described.
The key question here is : Can the above appear by pure chance or not? What do we need to make a claim that the above methodology works indeed ? From what I understand a key part is to find the number of plausible topics for MECFS and then run an appropriate analysis. I find it extremely hard that this can reliably take place but I am open to any suggestions. I can provide a full list of identified concepts from my part.
If this is cherry picking then I see no harm done apart from wasting 15 years of my life in trying to convince others but at least I can now function and have a near-normal life. So harm for my time (and income) but no harm for the patient's health and wallets.
But if indeed is something taking place here then we are talking about negative bias consistently over the years. Can patients "afford" not to look at this methodology? @forestglip @Hutan also would appreciate your input.