Preliminary thoughts on this study - the reduction in VO2Peak on repeated CPET can only be due to one of two factors - the participant putting in less effort (as a participant in one of the studies I know this isn't the reason), or a reduction in blood volume circulating through the muscle. This is because VO2Max is limited by cardiovascular factors. We know it is not limited by mitochondrial capacity as motor unit recruitment is well below maximal at VO2Max.
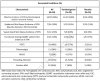
So Pyridostigmine should in principle help. But by how much? In this study, there was a 1% increase in VO2Peak in the Pyridostigmine group and a 3% reduction in the placebo group. Scraping in with a P=0.04.
Or in the Authors words:
The physiologic changes we describe are small and are not clinically relevant, but within groups are concordant and between groups are statistically significant.
The improved performance is indeed likely related to the improvement in right atrial pressure in the Pyridostigmine group.
The manuscript itself has some issues, the first is male participants were excluded due to a supposed randomisation error (this is a little suspicious). The participants reached VO2Peak at relatively low heart rates, well below expected age maximums and the VO2Peak figures were very low suggesting sub-maximal effort or very low levels of fitness.
They claim that the reduced performance is due to neurovascular dysregulation precipitated by prior exercise but provide a vague explanation as to how this could occur. They then try to claim that there is "increased sympathetic outflow in ME/CFS is supported by elevated plasma catecholamine levels and increased sympathetic nerve activity to the heart, skeletal muscle arterioles, and adrenals during rest". Despite the fact that studies of adults with ME/CFS has shown no difference in resting catecholamine levels and if there was too much sympathetic stimulation, the why would more sympathetic stimulation and hence venoconstriction be desirable (see their Figure 3 as the proposed mechanism - "cholinergic stimulation of
norepinephrine release at the post-ganglionic synapse").
Edit even for OI patients, as far back as 1988, it was known that patients have normal norepinephrine levels at rest, an it is upon orthostatic stress that any increased sympathetic stimulation is a response to venous pooling:
https://europepmc.org/article/MED/3343547
The manuscript then claims that there is evidence of hyperventilation in this group, but that is not true - the mean VE/VCO2 and VD/VT of the participants are in the normal range for exercising individuals. If they wish to claim that a few patients were hyperventilating, they are going to have to provide more specific evidence - how many reached a particular threshold for the various measures for example.
They then cite the Bohr effect without understanding that the Bohr effect is fairly small at physiological pressures in humans. Their reference is a prior Systrom study (that I had previously commented on), but that study does not provide any basis for claims about the importance of the Bohr effect, in fact the
study they cite has the opposite conclusion.
No evidence was observed for over-ventilation of CO2, causing the arterial blood to become more alkaline during exercise in the patient groups studied.
This is despite the fact that some of the patient groups in that study had much higher VE/VCO2 slopes compared to the ME/CFS patients in the study of Systrom et al.