LarsSG
Senior Member (Voting Rights)
Background: Some patients with acute COVID-19 are left with persistent, debilitating fatigue, cognitive impairment (“brain fog”), orthostatic intolerance (OI) and other symptoms (“Long COVID”). Many of the symptoms are like those of other post-infectious fatigue syndromes and may meet criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Common diagnostic laboratory tests are often unrevealing.
Methods: We evaluated whether a simple, standardized, office-based test of OI, the 10-min NASA Lean Test (NLT), would aggravate symptoms and produce objective hemodynamic and cognitive abnormalities, the latter being evaluated by a simple smart phone-based app.
Participants: People with Long COVID (N = 42), ME/CFS (N = 26) and healthy control subjects (N = 20) were studied just before, during, immediately after, 2 and 7 days following completion of the NLT.
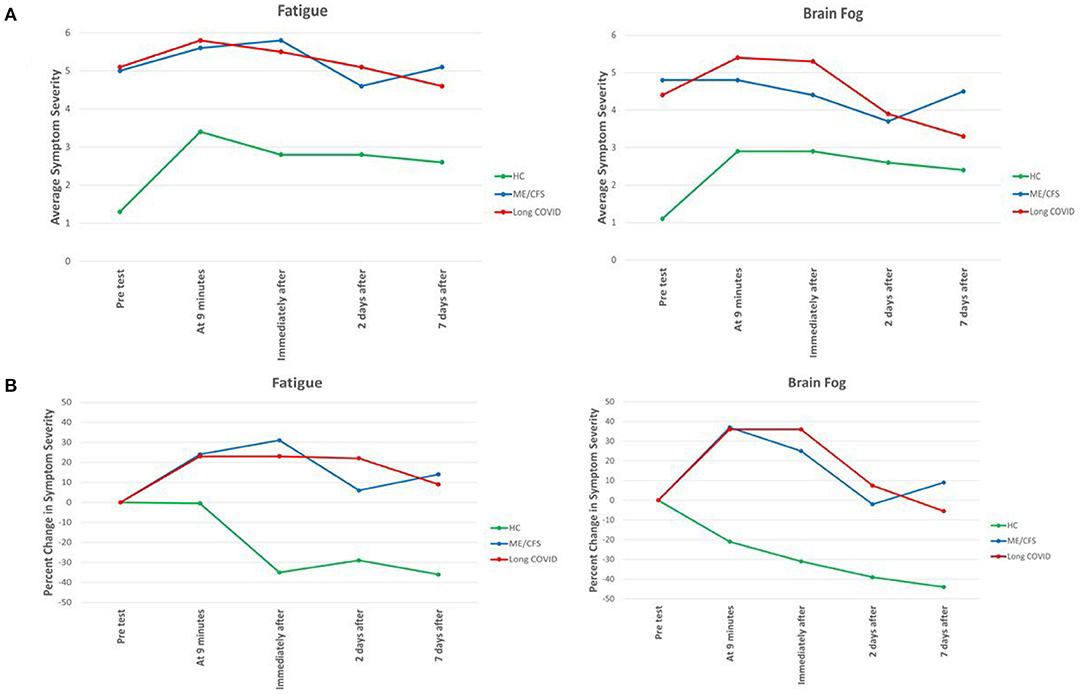
Results: The NLT provoked a worsening of symptoms in the two patient groups but not in healthy control subjects, and the severity of all symptoms was similar and significantly worse in the two patient groups than in the control subjects (p < 0.001). In the two patient groups, particularly those with Long COVID, the NLT provoked a marked and progressive narrowing in the pulse pressure. All three cognitive measures of reaction time worsened in the two patient groups immediately following the NLT, compared to the healthy control subjects, particularly in the Procedural Reaction Time (p < 0.01).
Conclusions: A test of orthostatic stress easily performed in an office setting reveals different symptomatic, hemodynamic and cognitive abnormalities in people with Long COVID and ME/CFS, compared to healthy control subjects. Thus, an orthostatic challenge easily performed in an office setting, and the use of a smart phone app to assess cognition, can provide objective confirmation of the orthostatic intolerance and brain fog reported by patients with Long COVID and ME/CFS.
Full text
Methods: We evaluated whether a simple, standardized, office-based test of OI, the 10-min NASA Lean Test (NLT), would aggravate symptoms and produce objective hemodynamic and cognitive abnormalities, the latter being evaluated by a simple smart phone-based app.
Participants: People with Long COVID (N = 42), ME/CFS (N = 26) and healthy control subjects (N = 20) were studied just before, during, immediately after, 2 and 7 days following completion of the NLT.
Results: The NLT provoked a worsening of symptoms in the two patient groups but not in healthy control subjects, and the severity of all symptoms was similar and significantly worse in the two patient groups than in the control subjects (p < 0.001). In the two patient groups, particularly those with Long COVID, the NLT provoked a marked and progressive narrowing in the pulse pressure. All three cognitive measures of reaction time worsened in the two patient groups immediately following the NLT, compared to the healthy control subjects, particularly in the Procedural Reaction Time (p < 0.01).
Conclusions: A test of orthostatic stress easily performed in an office setting reveals different symptomatic, hemodynamic and cognitive abnormalities in people with Long COVID and ME/CFS, compared to healthy control subjects. Thus, an orthostatic challenge easily performed in an office setting, and the use of a smart phone app to assess cognition, can provide objective confirmation of the orthostatic intolerance and brain fog reported by patients with Long COVID and ME/CFS.
Full text