Edit: Paper now published
Post with abstract here.
Outpatient Treatment of COVID-19 and the Development of Long COVID Over 10 Months: A Multi-Center, Quadruple-Blind, Parallel Group Randomized Phase 3 Trial
Link (Open access to full paper)
**************
Preprint abstract
Outpatient treatment of Covid-19 with metformin, ivermectin, and fluvoxamine and the development of Long Covid over 10-month follow-up
Background: Long Covid is an emerging chronic illness potentially affecting millions, sometimes preventing the ability to work or participate in normal daily activities. COVID-OUT was an investigator-initiated, multi-site, phase 3, randomized, quadruple-blinded placebo-controlled clinical trial (NCT04510194). The design simultaneously assessed three oral medications (metformin, ivermectin, fluvoxamine) using two by three parallel treatment factorial assignment to efficiently share placebo controls and assessed Long Covid outcomes for 10 months to understand whether early outpatient treatment of SARS-CoV-2 with metformin, ivermectin, or fluvoxamine prevents Long Covid.
Methods: This was a decentralized, remotely delivered trial in the US of 1,125 adults age 30 to 85 with overweight or obesity, fewer than 7 days of symptoms, and enrolled within three days of a documented SARS-CoV-2 infection. Immediate release metformin titrated over 6 days to 1,500mg per day 14 days total; ivermectin 430mcg/kg/day for 3 days; fluvoxamine, 50mg on day one then 50mg twice daily through 14 days. Medical-provider diagnosis of Long Covid, reported by participant by day 300 after randomization was a pre-specified secondary outcome; the primary outcome of the trial was severe Covid by day 14.
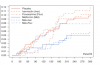
Result: The median age was 45 years (IQR 37 to 54), 56% female of whom 7% were pregnant. Two percent identified as Native American; 3.7% as Asian; 7.4% as Black/African American; 82.8% as white; and 12.7% as Hispanic/Latino. The median BMI was 29.8 kg/m2 (IQR 27 to 34); 51% had a BMI >30kg/m2. Overall, 8.4% reported having received a diagnosis of Long Covid from a medical provider: 6.3% in the metformin group and 10.6% in the metformin control; 8.0% in the ivermectin group and 8.1% in the ivermectin control; and 10.1% in the fluvoxamine group and 7.5% in the fluvoxamine control. The Hazard Ratio (HR) for Long Covid in the metformin group versus control was 0.58 (95% CI 0.38 to 0.88); 0.99 (95% CI 0.592 to 1.643) in the ivermectin group; and 1.36 in the fluvoxamine group (95% CI 0.785 to 2.385).
Conclusions: There was a 42% relative decrease in the incidence of Long Covid in the metformin group compared to its blinded control in a secondary outcome of this randomized phase 3 trial. Trial registration: NCT04510194; IND 152439
Link
Post with abstract here.
Outpatient Treatment of COVID-19 and the Development of Long COVID Over 10 Months: A Multi-Center, Quadruple-Blind, Parallel Group Randomized Phase 3 Trial
Link (Open access to full paper)
**************
Preprint abstract
Outpatient treatment of Covid-19 with metformin, ivermectin, and fluvoxamine and the development of Long Covid over 10-month follow-up
Carolyn T Bramante, John B Buse, David Liebovitz, Jacinda Nicklas, Michael A Puskarich, Ken Cohen, Hrishikesh Belani, Blake Anderson, Jared D Huling, Christopher Tignanelli, Jennifer Thompson, Matthew Pullen, Lianne Siegel, Jennifer Proper, David J Odde, Nichole Klatt, Nancy Sherwood, Sarah Lindberg, Esteban Lemus Wirtz, Amy Krager, Kenny Beckman, Spencer Erickson, Sarah Fenno, Katrina Hartman, Michael Rose, Barkha Patel, Gwendolyn Griffiths, Neeta Bhat, Thomas A Murray, David R Boulware
Background: Long Covid is an emerging chronic illness potentially affecting millions, sometimes preventing the ability to work or participate in normal daily activities. COVID-OUT was an investigator-initiated, multi-site, phase 3, randomized, quadruple-blinded placebo-controlled clinical trial (NCT04510194). The design simultaneously assessed three oral medications (metformin, ivermectin, fluvoxamine) using two by three parallel treatment factorial assignment to efficiently share placebo controls and assessed Long Covid outcomes for 10 months to understand whether early outpatient treatment of SARS-CoV-2 with metformin, ivermectin, or fluvoxamine prevents Long Covid.
Methods: This was a decentralized, remotely delivered trial in the US of 1,125 adults age 30 to 85 with overweight or obesity, fewer than 7 days of symptoms, and enrolled within three days of a documented SARS-CoV-2 infection. Immediate release metformin titrated over 6 days to 1,500mg per day 14 days total; ivermectin 430mcg/kg/day for 3 days; fluvoxamine, 50mg on day one then 50mg twice daily through 14 days. Medical-provider diagnosis of Long Covid, reported by participant by day 300 after randomization was a pre-specified secondary outcome; the primary outcome of the trial was severe Covid by day 14.
Result: The median age was 45 years (IQR 37 to 54), 56% female of whom 7% were pregnant. Two percent identified as Native American; 3.7% as Asian; 7.4% as Black/African American; 82.8% as white; and 12.7% as Hispanic/Latino. The median BMI was 29.8 kg/m2 (IQR 27 to 34); 51% had a BMI >30kg/m2. Overall, 8.4% reported having received a diagnosis of Long Covid from a medical provider: 6.3% in the metformin group and 10.6% in the metformin control; 8.0% in the ivermectin group and 8.1% in the ivermectin control; and 10.1% in the fluvoxamine group and 7.5% in the fluvoxamine control. The Hazard Ratio (HR) for Long Covid in the metformin group versus control was 0.58 (95% CI 0.38 to 0.88); 0.99 (95% CI 0.592 to 1.643) in the ivermectin group; and 1.36 in the fluvoxamine group (95% CI 0.785 to 2.385).
Conclusions: There was a 42% relative decrease in the incidence of Long Covid in the metformin group compared to its blinded control in a secondary outcome of this randomized phase 3 trial. Trial registration: NCT04510194; IND 152439
Link
Last edited by a moderator: