You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Patient-Reported Treatment Outcomes in ME/CFS and Long COVID, 2024, Eckey, Davis, Xiao+
- Thread starter SNT Gatchaman
- Start date
wingate
Senior Member (Voting Rights)
I haven’t read the paper, but what stood out to me was the information in Figure 2, and particularly how the efficacy of various treatments compared to the efficacy of pacing, a treatment that the majority of respondents said was at least slightly helpful.
In my experience, lack of pacing is very likely to make my symptoms worse, but even strict pacing hasn’t made my symptoms improve over time.
So, even if there were several “helpful” treatments, but they were only as helpful as pacing, then none on this list in fig. 2 would seem to be too promising to me.
In my experience, lack of pacing is very likely to make my symptoms worse, but even strict pacing hasn’t made my symptoms improve over time.
So, even if there were several “helpful” treatments, but they were only as helpful as pacing, then none on this list in fig. 2 would seem to be too promising to me.
This.In my experience, lack of pacing is very likely to make my symptoms worse, but even strict pacing hasn’t made my symptoms improve over time.
Pacing certainly helped with an initial and welcome improvement, but I quickly hit a ceiling that has never gone away. Beyond that it mostly has just helped slow down the rate of deterioration.
But it is still a very unsatisfactory outcome overall.
Ignoring improvement and just comparing totals for any worsening category: much worse, moderately worse, slightly worse —
GET (162 + 57 + 27) / 299 = 82%, 54% being "much worse" (ME = 263, LC = 36)
Pacing (10 + 9 + 9) / 803 = 2.2%, 1.2% being "much worse" (ME = 684, LC = 119)
GET (162 + 57 + 27) / 299 = 82%, 54% being "much worse" (ME = 263, LC = 36)
Pacing (10 + 9 + 9) / 803 = 2.2%, 1.2% being "much worse" (ME = 684, LC = 119)
Sasha
Senior Member (Voting Rights)
I've just come across this survey. Obviously it can't offer strong conclusions about what works - it wasn't a collection of randomised trials on therapies - but does it offer even an approximate indication of which therapies might be worth prioritising for RCTs, or which theories of ME/CFS might be on the right track?
I don't think it's useful. My memory of the data collection was that it was largely promoted on Twitter as part of the early enthusiasm among people with Long Covid who were excitedly sharing their experiments with all sorts of treatments and egging each other on. Many were trying multiple things at the same time and claiming success after very brief experiments that were probably just random fluctuations.
There also seems to be the same issues which I find hard to explain succinctly (and pacing in concept is better than GET obviously) but is along the lines of:I haven’t read the paper, but what stood out to me was the information in Figure 2, and particularly how the efficacy of various treatments compared to the efficacy of pacing, a treatment that the majority of respondents said was at least slightly helpful.
In my experience, lack of pacing is very likely to make my symptoms worse, but even strict pacing hasn’t made my symptoms improve over time.
So, even if there were several “helpful” treatments, but they were only as helpful as pacing, then none on this list in fig. 2 would seem to be too promising to me.
the wrong message tends to be the take-away of too many, certainly those without ME, from suggestions that pacing helps: they think it is the strict routine and 'behaving oneself' that makes the difference, rather than wanting to take on board it is the reduction in committments that one must try and juggle/be responsible for. Within that second bit there is probably some points for the 'doing less' part but if you have just as much hanging over you on your plate then translating that into the doing less still has lots of hidden costs regarding cognitive load, pressures, displeased people or living in a pigsty that will eventually turn into an avalanche etc.
As being able to do said pacing routine probably has as default having a to-do list that can fit into the week then it is hard to be sure it is one and not the other when those who might end up actually more well than they started out but still sleeping at funny times or having a day of 'doing stuff' then two days of crashing or taking it very easy (and then having the energy for the next thing) might.
And of course that's a problem because the cherry-pickers are then allowed to think it was the early night that helped, or 'pacing' in a marathon sense, and not people were able to sleep at x time because they didn't have to overdo it during the day or 'having less to fit in'.
The second part is what most other trials on the behavioural front that aren't eg retrospective or open looking at people's natural behaviour - and that is that 'those who it fits best anyway, or are well enough and/or getting weller will be the ones who can stick with a regimen and those who are more unwell can't and will have lots more appointments and unwell spells throwing out their chance of sticking to said prescribed routine'. SO whilst a less extreme Krypton factor filter it is acting as one none-the-less
Plus of course the energy for filling in anything is if you are getting worse or end up with some unexpected drama or task in your calendar perhaps one of the first non-essential things that would have to go if you were at the iller end (and already showering at the minimum) vs if you are in a position where situation vs threshold has more contingency.
Last edited:
Liie
Senior Member (Voting Rights)
I was curious what the score for CBT was in this survey.
I extracted it from Dataset S02.
CBT isn't as bad as GET. About as many people had a positive response as negative response, but those who were much worse were more numerous than those who were much better.
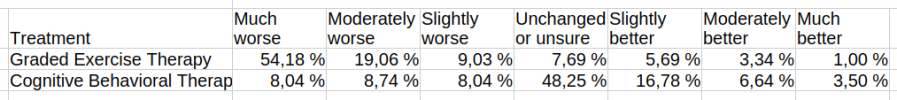
PS: I don't manage to paste table data from LibreOffice Calc here. The table looks good after pasting it but is transformed to source code when previewing.
I extracted it from Dataset S02.
CBT isn't as bad as GET. About as many people had a positive response as negative response, but those who were much worse were more numerous than those who were much better.
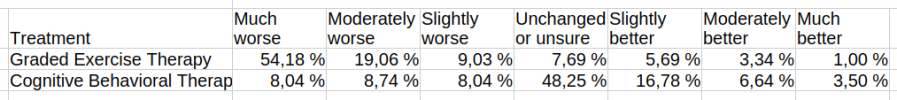
PS: I don't manage to paste table data from LibreOffice Calc here. The table looks good after pasting it but is transformed to source code when previewing.
To be fair that is interesting because it could either be that somehow for some people CBT was much easier to ignore/play the game with - which is what many assume, because if you are being made to actually 'do the GET' in the session 'it's different' than someone meddling with your thinking to get you to put aside pacing and think doing more is goodI was curious what the score for CBT was in this survey.
I extracted it from Dataset S02.
CBT isn't as bad as GET. About as many people had a positive response as negative response, but those who were much worse were more numerous than those who were much better.
View attachment 28979
PS: I don't manage to paste table data from LibreOffice Calc here. The table looks good after pasting it but is transformed to source code when previewing.
They've been trained to know they will receive an argument and a confrontational cognitive load of work and I assume a massive more amount of PEM from having their answer questioned if the therapist didn't like it 'what can you do more', 'why aren't you', 'you aren't doing your distraction/ignoring/why' vs if in-session you learn to comply and keep the therapist happy
Compared to GET when you are in a situation where someone is going to force you to do an xminute workout in the next GET session and saying 'I'm better for last time and felt great all week' isn't likely to make them more merciful so you have no choice but to log for the record you crawled around all week due to it.
But...
So many being stuck in the 'unsure' box jumps out to me because the whole point of the CBT is to mess-up people knowing what is north or south in their own bodies and to start feeling guilt if they acknowledge a symptom because they should see it as created by their 'giving it attention/mind' that it appears at all ie training in pretending, giving the right answers, gaslighting. How after that do you then manage to work out how you feel at all?
To them, if gaslighted to high heaven, what even is feeling worse or feeling better according to what is the right answer according to the therapist taught to be confrontational with them and what are they supposed to be feeling or seeing, what counts as doing because maybe the therapist keeps telling them they look more well and trying to congratulate them on having 'done x' and achieved things so they forget they are now spending 30secs brushing their teeth.
Being stuck in an out of body someone else controlling you people-pleasing mode where your ventriliquist doll has said 'something fake positive' for the pat on the head before you can even think and yet you now rely on deliveries and are struggling to shower enough ie function has gone down. But hey 'I'm talking positive, so... is that the 'feeling better'?'
They've just spent the last however many weeks being coerced and controlled even when the therapist isn't there by being forced to say these things lest they get what is a deliberate massive confrontation (which might just as well have been designed to use someone's disability to attack their mental health and very core of who they are and make them question their own reality) - when they have an illness where that exertion in itself they know causes both hurt personally, deeply when newly diagnosed are vulnerable and needing support in their identity and physically because being shouted at and required to 'explain yourself' is abuse and a lot of energy noone likes - and it aint the helpful type of questioning people lie 'like if a non-pwme had cbt' (because BACME and other bps now bang on about their bs 'stress reduction' and 'it's not caused by but it is persistent due to stress').
After enough of those dressing downs I imagine its very much like a coercive relationship where to avoid the huge PEM and if already with cognitive and physical fatigue/fatiguability you have to avoid getting into something that other person simply is deliberately not going to hear logic on because they are instructed and/or trained to believe nonsense and put a hand up and say 'talk to the hand' until you say the right thing.
It's literal brainwashing conditions to be frank, but combined with almost having a relationship with someone 'not healthy for you' (there are other straightforward words that are true also - people should not be being placed in these, but removed from such) - taking exhausted people, making them travel and sit somewhere they'll be uncomfortable because everywhere not bed or your own arrangement is when you have ME/CFS, and shooting their nerves by professionally losing your rag at certain answers and questioning them as wrong, whilst saying 'orrible things they are supposed to internalise and telling them they have to come back and if they report the same next time they'll get more of the same. How are they going to know their own answer, when keeping yourself safe now means prioritising what someone else's correct answer is.
And what is the safe answer for them to give. Work is going better even though they are doing less because whilst they are in treatment they are being given leeway, how is that going to change based on a therapist's letter etc. The fop of the 'I guess I feel slightly better then' feels explained by that awkward social pressure situation and other potential sources of coercion too.
The Heins et al (2013) info on CBT is a very interesting paper on this because it actually had objective activity and perceived activity. If you ignore their pseudophil (which is insight into how keen some are to find a way to think around logic in order to keep believing) it shows very simply that those who were most impacted by the CBT ie the 'fast responders' weren't actually doing any more than those who were non-responders. And none of them by the end were any different in objective activity
But also that those who were impacted by it thought they were less fatigued but it was simply because they thought they were doing more when actually they objectively weren't. ie the 'fatigue' they were being directed to assess was a backward calculation of how bad they felt after what they thought they'd done (rather than 'how bad they actually felt' and 'what their function meant they could objectively do'). A bit like expecting to feel suitably exhausted after your 5km park run, and noone telling you that's because you've been being allowed to think it was that but for the last 8weeks you've been doing a 4km course.
Last edited:
MrMagoo
Senior Member (Voting Rights)
I had the CBT of old, as an accompaniment to GET, the CbT was telling you to do GET.I was curious what the score for CBT was in this survey.
I extracted it from Dataset S02.
CBT isn't as bad as GET. About as many people had a positive response as negative response, but those who were much worse were more numerous than those who were much better.
View attachment 28979
PS: I don't manage to paste table data from LibreOffice Calc here. The table looks good after pasting it but is transformed to source code when previewing.
So basically I used to just lie because I thought it was nonsense, unscientific and unhelpful. “Why yes, I did walk an extra 5 minutes per day and I do feel better for pushing through!”
when you think of what is involved with getting it administered isn't just adding another tablet to whatever you might already have to take, then if medics understood how careful we have to be with exertion in one place meaning sacrifices elsewhere I would hope they would read these in that context.Yeah, oral fluids/electrolytes is pretty high too if looking at moderately improved. 23% of ME/CFS either moderately or much improved. It also has the highest number of people who answered out of the 181 treatments.
View attachment 24723
SOmeone is aware 'much better' might be read as your ME has somehow gone, so moderately better means 'a lot' given the context of how much disability could be improved whilst still having a lot more disability than anyone would imagine. And slightly better mightn't seem 'much' to other people or even other illnesses but given the breadline of threshold we are on vs the committments then having a 10% improvement could mean being able to sit up for hours in a day where previously it was touch and go if you could at all. Or social contact. Or getting teeth brushed enough they don't rot and showered enough you don't get other issues.
And all those are 'factoring in' what it takes to get the therapy. I'd imagine the 'unsures' are balancing whether what is involved with it is 'worth it' on balance. ie the overall. ?
but even if done at home there will be significantly more exertion, and I imagine other pwme would be like me where I can get significant pain even from blood tests up and down the arm for quite a while
for those most ill even if done lying in bed then the presence of another person and noise etc.
for those less ill the having to dress and perhaps sit up and be ready on time without being too unhygienic (washed and teeth brushed recently)
if home visit making sure the part of the home isn't a flea pit which even if done by someone else means noise and disturbance
for those travelling somewhere then all that re: getting ready, plus travel, plus sitting uncomfortably during it
CBT in the USA is different from CBT in UKTo be fair that is interesting because it could either be that somehow for some people CBT was much easier to ignore/play the game with - which is what many assume, because if you are being made to actually 'do the GET' in the session 'it's different' than someone meddling with your thinking to get you to put aside pacing and think doing more is good
They've been trained to know they will receive an argument and a confrontational cognitive load of work and I assume a massive more amount of PEM from having their answer questioned if the therapist didn't like it 'what can you do more', 'why aren't you', 'you aren't doing your distraction/ignoring/why' vs if in-session you learn to comply and keep the therapist happy
Compared to GET when you are in a situation where someone is going to force you to do an xminute workout in the next GET session and saying 'I'm better for last time and felt great all week' isn't likely to make them more merciful so you have no choice but to log for the record you crawled around all week due to it.
But...
So many being stuck in the 'unsure' box jumps out to me because the whole point of the CBT is to mess-up people knowing what is north or south in their own bodies and to start feeling guilt if they acknowledge a symptom because they should see it as created by their 'giving it attention/mind' that it appears at all ie training in pretending, giving the right answers, gaslighting. How after that do you then manage to work out how you feel at all?
To them, if gaslighted to high heaven, what even is feeling worse or feeling better according to what is the right answer according to the therapist taught to be confrontational with them and what are they supposed to be feeling or seeing, what counts as doing because maybe the therapist keeps telling them they look more well and trying to congratulate them on having 'done x' and achieved things so they forget they are now spending 30secs brushing their teeth.
And what is the safe answer for them to give. Work is going better even though they are doing less because whilst they are in treatment they are being given leeway, how is that going to change based on a therapist's letter etc. The fop of the 'I guess I feel slightly better then' feels explained by that awkward social pressure situation and other potential sources of coercion too.
The Heins et al (2013) info on CBT is a very interesting paper on this because it actually had objective activity and perceived activity. If you ignore their pseudophil (which is insight into how keen some are to find a way to think around logic in order to keep believing) it shows very simply that those who were most impacted by the CBT ie the 'fast responders' weren't actually doing any more than those who were non-responders. And none of them by the end were any different in objective activity
But also that those who were impacted by it thought they were less fatigued but it was simply because they thought they were doing more when actually they objectively weren't. ie the 'fatigue' they were being directed to assess was a backward calculation of how bad they felt after what they thought they'd done (rather than 'how bad they actually felt' and 'what their function meant they could objectively do'). A bit like expecting to feel suitably exhausted after your 5km park run, and noone telling you that's because you've been being allowed to think it was that but for the last 8weeks you've been doing a 4km course.
Do we actually know what the content of the CBT was that each of those filling in the survey was and the 'bent' of the person delivering it ?CBT in the USA is different from CBT in UK
It would be interesting to know if reliably in the USA someone got someone who understood long covid (and/or me/cfs) in the way we do rather than the old-school bps/bacme type or feigning they get it is exhausting but are somewhere in the middle thinking 'but you can make an effort to try and slowly do more' etc.
CBT in USA tends to be more like the original Beck type, not so much the " curative" type . This may of course vary per provider. I have a friend who did her Psychology PhD in the US who commented on the difference when I queried it years ago.Do we actually know what the content of the CBT was that each of those filling in the survey was and the 'bent' of the person delivering it ?
It would be interesting to know if reliably in the USA someone got someone who understood long covid (and/or me/cfs) in the way we do rather than the old-school bps/bacme type or feigning they get it is exhausting but are somewhere in the middle thinking 'but you can make an effort to try and slowly do more' etc.
Peter T
Senior Member (Voting Rights)
I do wonder
That is interesting, because the PACE type CBT advocated for by such as Wessely and Chalder seems totally at odds with the principles of CBT as I was taught them as a psychology undergraduate in the UK in the 1970s. The whole point of CBT was that it was to give individuals tools to change their behaviour that were neutral in terms of any theories or beliefs about aetiology, with it being non directive, the aims being agreed by both the client and the clinician, not dictated by the clinician.
Though even then it is problematic with a biomedical condition, where it does not matter, even if the client wants to do more, as the limiting factor is their condition not their thinking. It makes as much sense using CBT to try to reduce gravity or change the speed of light. However it does at least make theoretical sense to use CBT to help someone with ME/CFS, if they perceive a need, to reduce their activity to levels sustainable in line with the limitations imposed by their condition.
[added - perhaps a good analogy to PACE type CBT might be that someone wanting to reduce their weight is advised to have CBT aimed at reducing the amount of gravity their body experiences.]
CBT in USA tends to be more like the original Beck type, not so much the " curative" type . This may of course vary per provider. I have a friend who did her Psychology PhD in the US who commented on the difference when I queried it years ago.
That is interesting, because the PACE type CBT advocated for by such as Wessely and Chalder seems totally at odds with the principles of CBT as I was taught them as a psychology undergraduate in the UK in the 1970s. The whole point of CBT was that it was to give individuals tools to change their behaviour that were neutral in terms of any theories or beliefs about aetiology, with it being non directive, the aims being agreed by both the client and the clinician, not dictated by the clinician.
Though even then it is problematic with a biomedical condition, where it does not matter, even if the client wants to do more, as the limiting factor is their condition not their thinking. It makes as much sense using CBT to try to reduce gravity or change the speed of light. However it does at least make theoretical sense to use CBT to help someone with ME/CFS, if they perceive a need, to reduce their activity to levels sustainable in line with the limitations imposed by their condition.
[added - perhaps a good analogy to PACE type CBT might be that someone wanting to reduce their weight is advised to have CBT aimed at reducing the amount of gravity their body experiences.]
Last edited:
I re-analyzed the n = 3,925 TREATME survey and wrote up the results.
Main methodological difference:
The original treats any improvement the same regardless if it's small or large. I instead calculated weighted average effect scores.
The top treatments are (on a scale of -5.0 to 5.0):
Omalizumab/Xolair: 0.69 - 4.22 (not significant)
IV Saline: 1.84 - 2.14
Maraviroc:1.23 - 2.30
Ketamine: 0.93 - 2.40
Enoxaparine or unfractionated heparin: 1.00 - 2.29
Ivabradine: 1.29 - 1.85
Some of these could still use a trial. However, I also think that perhaps the biggest value of this survey is that a lot of lower vamos treatments can be "crossed off the list" and that researchers should explicitly trial drugs not on this list.
You can read the full piece on my Substack!
https://open.substack.com/pub/viralpersistence/p/re-analyzing-the-treatme-survey
I want to thank Martha Eckey (LongCovidPharmD) for collecting such a great dataset and making it available for analysis.
Main methodological difference:
The original treats any improvement the same regardless if it's small or large. I instead calculated weighted average effect scores.
The top treatments are (on a scale of -5.0 to 5.0):
Omalizumab/Xolair: 0.69 - 4.22 (not significant)
IV Saline: 1.84 - 2.14
Maraviroc:1.23 - 2.30
Ketamine: 0.93 - 2.40
Enoxaparine or unfractionated heparin: 1.00 - 2.29
Ivabradine: 1.29 - 1.85
Some of these could still use a trial. However, I also think that perhaps the biggest value of this survey is that a lot of lower vamos treatments can be "crossed off the list" and that researchers should explicitly trial drugs not on this list.
You can read the full piece on my Substack!
https://open.substack.com/pub/viralpersistence/p/re-analyzing-the-treatme-survey
I want to thank Martha Eckey (LongCovidPharmD) for collecting such a great dataset and making it available for analysis.
Attachments
There is a mention that publication bias effects results of papers on treatments and that this is not the case for this approach but fails to mention that this approach suffers from other problems such as popularity bias, which in certain instances is just a result of publication bias and even worse phenomena.
Given the natural high (enough) recovery rates, or at least reported improvements in the conditions of these people, one should expect that a weighted approach would be beneficial to several substances with no efficacy especially when several treatments were only tested in few individuals. For example giving placebo long enough to the people in the intramural trial would have resulted in a full remission in 4/17 (and here the problems will be even worse due to the lack of any accurate diagnosis assessment and no minimum length of illness duration).
Given the natural high (enough) recovery rates, or at least reported improvements in the conditions of these people, one should expect that a weighted approach would be beneficial to several substances with no efficacy especially when several treatments were only tested in few individuals. For example giving placebo long enough to the people in the intramural trial would have resulted in a full remission in 4/17 (and here the problems will be even worse due to the lack of any accurate diagnosis assessment and no minimum length of illness duration).
One would like to think so but then because there's zero rigor in assessing what different conditions all of these people had or how treament was assessed (incl. dosages ect) maybe not even that can be said."However, I also think that perhaps the biggest value of this survey is that a lot of lower vamos treatments can be "crossed off the list" and that researchers should explicitly trial drugs not on this list."
Collecting data like this with an online survey publicised on Twitter is bound to bring in masses of misinformation.
I can't remember all the details. We did discuss this survey when the results were published.
Did you take into account how long participants had used the drugs, what else they were trying at the same time, how long they had been ill, sample sizes for each drug, correction for multiple comparisons, subjective outcomes, and other confounding factors?
A lot of the participants had only been sick for a few months or at least less than 2 years with long covid. In that situation many will have been improving naturally anyway.
While it was an intersting attempt at data collection, I think the data is too compromised to draw useful conclusions.
I can't remember all the details. We did discuss this survey when the results were published.
Did you take into account how long participants had used the drugs, what else they were trying at the same time, how long they had been ill, sample sizes for each drug, correction for multiple comparisons, subjective outcomes, and other confounding factors?
A lot of the participants had only been sick for a few months or at least less than 2 years with long covid. In that situation many will have been improving naturally anyway.
While it was an intersting attempt at data collection, I think the data is too compromised to draw useful conclusions.



