Kalliope
Senior Member (Voting Rights)
JCI Insight
Plasma metabolomics reveals disrupted response and recovery following maximal exercise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Abstract
Post-exertional malaise (PEM) is a hallmark symptom of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
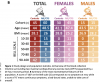
We monitored the evolution of 1,157 plasma metabolites in 60 ME/CFS cases (45 females, 15 males) and in 45 matched healthy control subjects (30 females, 15 males) before and after two maximal Cardiopulmonary Exercise Test (CPET) challenges separated by 24 hours, with the intent of provoking PEM in patients.
Four timepoints allowed exploration of the metabolic response to maximal energy-producing capacity and the recovery pattern of ME/CFS cases compared to the healthy control group.
Baseline comparison identified several significantly different metabolites, along with an enriched percentage of yet-to-be identified compounds.
Additionally, temporal measures demonstrated an increased metabolic disparity between cohorts, including unknown metabolites.
The effects of exertion in the ME/CFS cohort predominantly highlighted lipid- as well as energy-related pathways and chemical structure clusters, which were disparately affected by the first and second exercise sessions.
The 24-hour recovery period was distinct in the ME/CFS cohort, with over a quarter of the identified pathways statistically different.
The pathways that are uniquely different 24 hours after an exercise challenge provide clues to metabolic disruptions that lead to PEM.
Numerous altered pathways were observed to depend on glutamate metabolism, a crucial component to the homeostasis of many organs in the body, including the brain.
Plasma metabolomics reveals disrupted response and recovery following maximal exercise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Abstract
Post-exertional malaise (PEM) is a hallmark symptom of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
We monitored the evolution of 1,157 plasma metabolites in 60 ME/CFS cases (45 females, 15 males) and in 45 matched healthy control subjects (30 females, 15 males) before and after two maximal Cardiopulmonary Exercise Test (CPET) challenges separated by 24 hours, with the intent of provoking PEM in patients.
Four timepoints allowed exploration of the metabolic response to maximal energy-producing capacity and the recovery pattern of ME/CFS cases compared to the healthy control group.
Baseline comparison identified several significantly different metabolites, along with an enriched percentage of yet-to-be identified compounds.
Additionally, temporal measures demonstrated an increased metabolic disparity between cohorts, including unknown metabolites.
The effects of exertion in the ME/CFS cohort predominantly highlighted lipid- as well as energy-related pathways and chemical structure clusters, which were disparately affected by the first and second exercise sessions.
The 24-hour recovery period was distinct in the ME/CFS cohort, with over a quarter of the identified pathways statistically different.
The pathways that are uniquely different 24 hours after an exercise challenge provide clues to metabolic disruptions that lead to PEM.
Numerous altered pathways were observed to depend on glutamate metabolism, a crucial component to the homeostasis of many organs in the body, including the brain.