From the newest comment:
Also, as I highlighted before:
1. There's no baseline data, so they can't say there's no increase.
2. Even if they assume the groups were equal at baseline, a lack of increase in the percent of people with PEM only shows that people without PEM don't suddenly get it from exercise. It does not show that the intervention is safe for people who already have PEM.
They do have results for other PEM-related questions from the DePaul questionnaire that provide evidence that the intervention group is worse off than the standard care group at 3 months. I wonder why they didn't highlight these percentages in the paper.
I assume they meant there was no evidence of increased PEM. There was clearly evidence of PEM:Following analysis of the results by biostatisticians independent of the clinical research team, there was no evidence of post-exertional malaise (PEM) based on use of a validated questionnaire of PEM
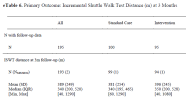
Of 99 individuals who completed the DePaul Symptom Questionnaire, 40 of 48 (83.3%) in the intervention group and 42 of 51 (82.4%) in the control group experienced postexertional malaise at 3-month follow-up (eTables 25-28 in Supplement 2).
Also, as I highlighted before:
1. There's no baseline data, so they can't say there's no increase.
2. Even if they assume the groups were equal at baseline, a lack of increase in the percent of people with PEM only shows that people without PEM don't suddenly get it from exercise. It does not show that the intervention is safe for people who already have PEM.
They do have results for other PEM-related questions from the DePaul questionnaire that provide evidence that the intervention group is worse off than the standard care group at 3 months. I wonder why they didn't highlight these percentages in the paper.
eTable 27. Post-Exertional Malaise at 3-Months, Part 2 (DePaul Symptom Questionnaire, Short Form) Additional Questions
If you were to become exhausted after actively participating in extracurricular activities, sports, or outings with friends, would you recover within an hour or two after the activity ended? (% for "No")
- Standard Care: 49.0%
- Intervention: 66.7%
Do you experience a worsening of your fatigue/energy related illness after engaging in minimal physical effort? (% for "Yes")
- Standard Care: 62.7%
- Intervention: 70.8%
Do you experience a worsening of your fatigue/energy related illness after engaging in minimal mental effort? (% for "Yes")
- Standard Care: 49.0%
- Intervention: 60.4%
Last edited: