- Home
- Forums
- ME/CFS and Long Covid news
- ME/CFS and Long Covid news
- Psychosomatic news - ME/CFS and Long Covid
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Swiss Re: Expert Forum on secondary COVID-19 impacts, Feb 2021
- Thread starter Sly Saint
- Start date
Kalliope
Senior Member (Voting Rights)
Sly Saint
Senior Member (Voting Rights)
Video of the presentation posted on another thread
"This is the video of Michael Sharpe's presentation on Long COVID to Swiss Re. It may have been removed from their website now, but, fortunately, it's been uploaded to a file-sharing site, in order that such an extraordinary contribution to medical history can be archived for posterity!"
"This is the video of Michael Sharpe's presentation on Long COVID to Swiss Re. It may have been removed from their website now, but, fortunately, it's been uploaded to a file-sharing site, in order that such an extraordinary contribution to medical history can be archived for posterity!"
Invisible Woman
Senior Member (Voting Rights)
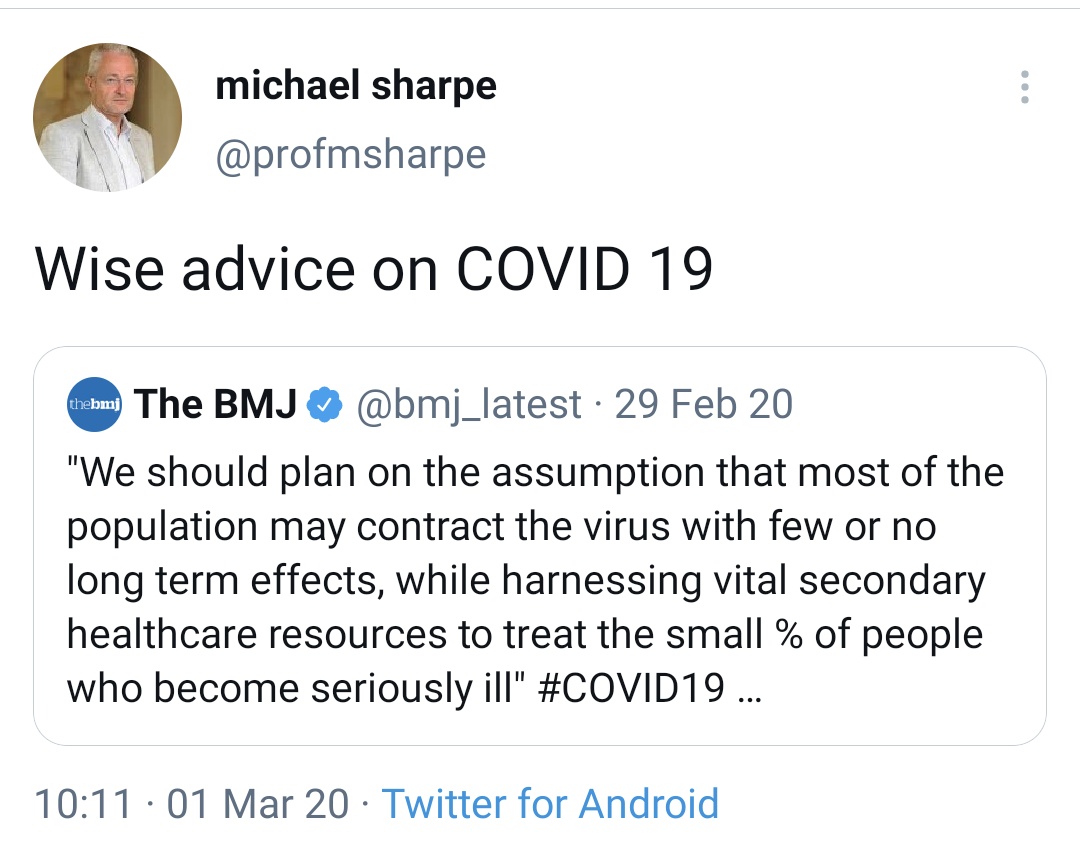
George Monbiot's tweet
I think that's the wrong question. Here are some alternatives -
1. What is it worth to them to carry on denying the suffering of hundreds of thousands of people in the UK & millions worldwide?
2. In these "woke" times how long will the business model of denial of suffering and stigmatizing some of the most vulnerable in society continue?
3. Psychiatrists like Sharpe & Wessely plus other mental health care professionals like Chalder work with many extremely vulnerable people. They have a history stigmatizing the patient and denying their illness. Where is the oversight to stop this continuing?
I wonder whether the people who so airily dismiss Long Covid, ME and CFS as "psychosomatic" or "imaginary" have any idea of how real and horrible is the suffering experienced by so many people with these conditions, or of how desperately they try to recover.
I think that's the wrong question. Here are some alternatives -
1. What is it worth to them to carry on denying the suffering of hundreds of thousands of people in the UK & millions worldwide?
2. In these "woke" times how long will the business model of denial of suffering and stigmatizing some of the most vulnerable in society continue?
3. Psychiatrists like Sharpe & Wessely plus other mental health care professionals like Chalder work with many extremely vulnerable people. They have a history stigmatizing the patient and denying their illness. Where is the oversight to stop this continuing?
Looks like awareness of this is growing in the LC community. Darren is (or part of) Long Covid Physio.
I think they've badly underestimated the difference between gaslighting LongCovid and M.E. patients. Using the same old tired, discredited arguments against a vast group of people who are largely in contact with each other and all got ill at roughly the same time is not going to work this time. It's quite sad and pathetic really.
Wyva
Senior Member (Voting Rights)
This is something I really would like to think. But I'm also kind of worried because in the last few weeks I've seen some long haulers saying things like "it also depends on if you want to get better - because some people just don't", "the mindset matters a lot", "you have to get back to being active, the symptoms will disappear after a while" etc.I think they've badly underestimated the difference between gaslighting LongCovid and M.E. patients. Using the same old tired, discredited arguments against a vast group of people who are largely in contact with each other and all got ill at roughly the same time is not going to work this time. It's quite sad and pathetic really.
Yesterday I saw an article in a popular women's magazine here, where the author used to be a long hauler and he said stuff like: "if you are physically able, you have to get off the couch and push yourself to go out and do things, no matter how week you feel or how little motivation you have". He equated brainfog with a state of lack of motivation and feeling hopeless. These are long haulers or former long haulers and this worries me. I don't know if they just repeat what their doctors told them or they came up with this themselves. (Or if they have the ME/CFS-like long covid and not some other sequelae.)
(I could mention that no one said anything like this in the glandular fever forums I frequented in my first 1-2 years and where almost everyone had post-viral fatigue syndrome, and people with acute cases were really rare, so it was basically a "long mono" group. Everyone was convinced there that the symptoms are real, however that forum was smaller than the LC groups, so it may be due to simple statistics and not something else.)
On the flipside: there are definitely long haulers who are adamant about this not being a psychosomatic issue.
Wonko
Senior Member (Voting Rights)
In a legal case wouldn't they just call an 'expert' witness in their defense? They only have to show that they acted in accord with 'best practice' and as they direct that......If one, or a group of individuals is blamed for causing, generating, supporting, and/or aiding the continuance of a devastating disease, what might the legal ramifications of this be? Hmmmm....
Good point @ Wonko. This would appear to be a likely scenario in a legal situation. Maligning whole groups could be explained as "best practice".
On another note, journalists daren't write about anything of concern, e.g. wars, disease, widespread financial collapse, for fear of being blamed for causing these catastrophes.


On another note, journalists daren't write about anything of concern, e.g. wars, disease, widespread financial collapse, for fear of being blamed for causing these catastrophes.
rvallee
Senior Member (Voting Rights)
One thing I think should be mentioned: this is Sharpe's main career focus, he has spent decades "studying" this, wrote books and academic/clinical chapters, taught it as a professor, was gifted millions to pursue his expertise, publishing dozens of papers, presenting to professional audiences and more.
And this presentation, entirely devoid of substance, relying on a combination of circular logical fallacies, anecdotes and innuendo, is essentially a full summary of the extent of his knowledge on the issue. In presenting the sum of his career's work to a professional audience, likely paid, this is the best he can do.
There is nothing of substance in this presentation. It's entirely vague and contains no expert knowledge whatsoever. And still, it actually represents the actual sum of the knowledge this "expert" has on his main topic of expertise. I'm sure he could ramble on for hours elaborating but there would still be no substance there, only more rhetoric and sophistry.
And this pathetic accumulation of ignorance has ruined millions of lives. It's truly unbelievable when the facts are simply stated.
And this presentation, entirely devoid of substance, relying on a combination of circular logical fallacies, anecdotes and innuendo, is essentially a full summary of the extent of his knowledge on the issue. In presenting the sum of his career's work to a professional audience, likely paid, this is the best he can do.
There is nothing of substance in this presentation. It's entirely vague and contains no expert knowledge whatsoever. And still, it actually represents the actual sum of the knowledge this "expert" has on his main topic of expertise. I'm sure he could ramble on for hours elaborating but there would still be no substance there, only more rhetoric and sophistry.
And this pathetic accumulation of ignorance has ruined millions of lives. It's truly unbelievable when the facts are simply stated.
Invisible Woman
Senior Member (Voting Rights)
Yesterday I saw an article in a popular women's magazine here, where the author used to be a long hauler and he said stuff like: "if you are physically able, you have to get off the couch and push yourself to go out and do things, no matter how week you feel or how little motivation you have". He equated brainfog with a state of lack of motivation and feeling hopeless. These are long haulers or former long haulers and this worries me. I don't know if they just repeat what their doctors told them or they came up with this themselves. (Or if they have the ME/CFS-like long covid and not some other sequelae.)
Ah but there's a big difference between someone who can get up and get their behind off the sofa, even if it feels very difficult and they're tired and not in the mood, and someone who can only do this once, twice or not at all.
I've experienced bouts of illness that have left me too weak to stand long before I got ME. As a youngster I was up and running about in no time.
As an adult, even a young adult it is harder because you have other commitments - exams, work etc. So it may take longer and regaining fitness does take effort and motivation.
That is not the same thing at all as having ME. I daresay for many with long covid it won't be the same thing either. If you are able to get off that couch and slowly regain your stamina and health then by definition you do not have the same thing. It really is that simple.
Comparing yourself to someone suffering from ME or long covid that is ME-like is like an Olympian athlete wondering why you, as a healthy person, can't compete with them as a chosen sport.
It's a nonsense.
One thing I think should be mentioned: this is Sharpe's main career focus, he has spent decades "studying" this, wrote books and academic/clinical chapters, taught it as a professor, was gifted millions to pursue his expertise, publishing dozens of papers, presenting to professional audiences and more.
And this presentation, entirely devoid of substance, relying on a combination of circular logical fallacies, anecdotes and innuendo, is essentially a full summary of the extent of his knowledge on the issue. In presenting the sum of his career's work to a professional audience, likely paid, this is the best he can do.
There is nothing of substance in this presentation. It's entirely vague and contains no expert knowledge whatsoever. And still, it actually represents the actual sum of the knowledge this "expert" has on his main topic of expertise. I'm sure he could ramble on for hours elaborating but there would still be no substance there, only more rhetoric and sophistry.
And this pathetic accumulation of ignorance has ruined millions of lives. It's truly unbelievable when the facts are simply stated.
Bravo!
rvallee
Senior Member (Voting Rights)
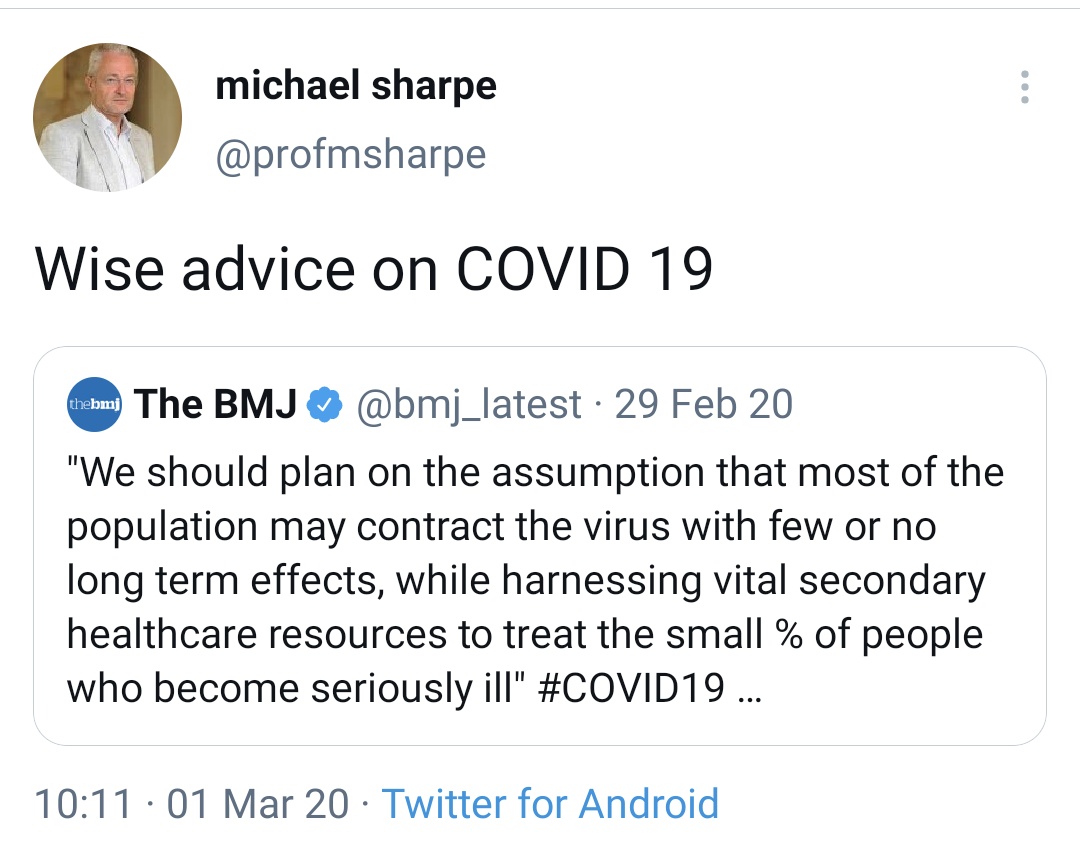
Turns out it's actually worse than this, a "world-leading expert" on the topic of post-infectious illness literally did not see the obvious coming, the obvious that much of the patient community did predict and warn about, as well as the actual experts that this ignoramus dismisses.
Turns out that fake expertise is indeed entirely fake and of no value whatsoever in itself. In this case Sharpe is doing exactly the only value his quackery has ever had: provide insurers with implausible cover the same way the scientists working with the tobacco industry to kill people for profit did.
Turns out that fake expertise is indeed entirely fake and of no value whatsoever in itself. In this case Sharpe is doing exactly the only value his quackery has ever had: provide insurers with implausible cover the same way the scientists working with the tobacco industry to kill people for profit did.
I don't have any medical training; perhaps others with expertise in the area of lung disease etc., may wish to comment.
Did I hear correctly on the presentation:
Fibrosis from COVID is reversible?
This article doesn't seem to paint such a definite picture:

Indian J Tuberc. 2020 Nov 10
doi: 10.1016/j.ijtb.2020.11.003 [Epub ahead of print]
PMCID: PMC7654356
Post covid 19 pulmonary fibrosis- Is it reversible?
Deependra Kumar Rai,∗ Priya Sharma, and Rahul Kumar
Author information Article notes Copyright and License information Disclaimer
Go to:
Abstract
After the COVID-19 outbreak, increasing number of patients worldwide who have survived COVID-19 continue to battle the symptoms of the illness, long after they have been clinically tested negative for the disease. As we battle through this pandemic, the challenging part is to manage COVID-19 sequelae which may vary from fatigue and body aches to lung fibrosis. This review addresses underlying mechanism, risk factors, course of disease and treatment option for post covid pulmonary fibrosis. Elderly patient who require ICU care and mechanical ventilation are at the highest risk to develop lung fibrosis. Currently, no fully proven options are available for the treatment of post inflammatory COVID 19 pulmonary fibrosis.
3. Conclusion
Considering huge numbers of individuals affected by COVID-19, even rare complications like post covid pulmonary fibrosis will have major health effects at the population level. Elderly patient who require ICU care and mechanical ventilation are the highest risk to develop lung fibrosis. Currently, no fully proven options are available for the treatment of post inflammatory COVID 19 pulmonary fibrosis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7654356/
ETA: Thank you @Esther12 for the transcript of this talk.
From the transcript re fibrosis:
"the main imaging abnormalities are just
um chest x-ray and chest ct
where you generally see resolving
fibrosis and that's
that's the main abnormalities that we see"
ETA #2:
From this same study -
"Many studies have shown that most common abnormality of lung function in discharged survivors with COVID-19 is impairment of diffusion capacity, followed by restrictive ventilatory defects, both associated with the severity of the disease21 , 22 Both decreased alveolar volume and K CO contribute to the pathogenesis of impaired diffusion capacity.23 At 3-months after discharge, residual abnormalities of pulmonary function were observed in 25.45% of the cohort which was lower than the abnormal pulmonary function in COVID-19 patients when discharged.10 Lung function abnormalities were detected in 14 out of 55 patients and the measurement of D-dimer levels at admission may be useful in prediction of impaired diffusion defect.16"
Did I hear correctly on the presentation:
Fibrosis from COVID is reversible?
This article doesn't seem to paint such a definite picture:

Indian J Tuberc. 2020 Nov 10
doi: 10.1016/j.ijtb.2020.11.003 [Epub ahead of print]
PMCID: PMC7654356
Post covid 19 pulmonary fibrosis- Is it reversible?
Deependra Kumar Rai,∗ Priya Sharma, and Rahul Kumar
Author information Article notes Copyright and License information Disclaimer
Go to:
Abstract
After the COVID-19 outbreak, increasing number of patients worldwide who have survived COVID-19 continue to battle the symptoms of the illness, long after they have been clinically tested negative for the disease. As we battle through this pandemic, the challenging part is to manage COVID-19 sequelae which may vary from fatigue and body aches to lung fibrosis. This review addresses underlying mechanism, risk factors, course of disease and treatment option for post covid pulmonary fibrosis. Elderly patient who require ICU care and mechanical ventilation are at the highest risk to develop lung fibrosis. Currently, no fully proven options are available for the treatment of post inflammatory COVID 19 pulmonary fibrosis.
3. Conclusion
Considering huge numbers of individuals affected by COVID-19, even rare complications like post covid pulmonary fibrosis will have major health effects at the population level. Elderly patient who require ICU care and mechanical ventilation are the highest risk to develop lung fibrosis. Currently, no fully proven options are available for the treatment of post inflammatory COVID 19 pulmonary fibrosis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7654356/
ETA: Thank you @Esther12 for the transcript of this talk.
From the transcript re fibrosis:
"the main imaging abnormalities are just
um chest x-ray and chest ct
where you generally see resolving
fibrosis and that's
that's the main abnormalities that we see"
ETA #2:
From this same study -
"Many studies have shown that most common abnormality of lung function in discharged survivors with COVID-19 is impairment of diffusion capacity, followed by restrictive ventilatory defects, both associated with the severity of the disease21 , 22 Both decreased alveolar volume and K CO contribute to the pathogenesis of impaired diffusion capacity.23 At 3-months after discharge, residual abnormalities of pulmonary function were observed in 25.45% of the cohort which was lower than the abnormal pulmonary function in COVID-19 patients when discharged.10 Lung function abnormalities were detected in 14 out of 55 patients and the measurement of D-dimer levels at admission may be useful in prediction of impaired diffusion defect.16"
Last edited:
Esther12
Senior Member (Voting Rights)
Video of the presentation posted on another thread
"This is the video of Michael Sharpe's presentation on Long COVID to Swiss Re. It may have been removed from their website now, but, fortunately, it's been uploaded to a file-sharing site, in order that such an extraordinary contribution to medical history can be archived for posterity!"
Auto-transcript part 1:
Transcript
so it's my great pleasure um to
introduce professor michael sharp
and i'll let him take over the screen
and share his slide deck but i'll tell
you a little bit about him
he's a professor of psychological
medicine at the university
at oxford university hospital um also
president of the academy of consultation
liaison psychiatry in the us
and vice president of the european
association of psychosomatic medicine
so that's a great cv and background to
talk to us today about postcovid
thank you thank you very much
um can you see my slides
we can thank you good excellent right
thank you so much
for inviting me um i i think maybe i'm
here for
a couple of main reasons
[Music]
one of them which is i've had a
career-long interest
in fatigue and the treatment of fatigue
but the other one is that i helped to
set up
our post covid clinic in oxford
which is based in the respiratory
department but which is
multidisciplinary and so i've i've had
some clinical experience of the kind of
patients that we're seeing
which i'm going to share with you um
given i'm giving the first talk in the
meeting i think it
might be important that we um at least
try and
agree what we're talking about uh not
entirely straightforward
um nice in the uk um
has offered us some definitions and as
you'll see
uh there's acute ongoing but it's
postcoded 19 at the bottom
that we're concerned about here
and this is setting a time of
12 weeks it doesn't specify any kind of
severity it just says signs and symptoms
and it does say not explained by another
diagnosis so this may not be universally
accepted
but we're working on people who have
significant symptoms
three months after an apparent infection
although those are not always documented
now i already heard this mentioned i'm
going to
intersperse my talk with some take away
messages
and one of them is it's been a tough
time for academics i can say as one
they've been stuck in their bedrooms
so what have they done they've done a
lot of internet surveys
and and that can give us some clues but
it's absolutely hopeless
uh giving us any kind of prevalence
estimates
and so uh because we never quite know
who denominator is it's just the people
that clicked on the questionnaire
so please be aware of this deluge of
poor quality research with unclear
denominators
there is some better research as you
heard coming down the track
so we all know about acute covid who
gets
so-called long-covid or becomes a long
hauler or post covered syndrome
everything i say is based on what's
published uh interpreted through
clinical and clinical uh experience
none of these are solid facts because
this is an evolving
evolving area of understanding but we're
probably thinking of five to ten percent
of patients at three months have some
kind of
severity of symptoms and disability many
more may
have lesser symptoms and lesser
disability they tend to be older
predominance of females and pre-morbid
vulnerability
asthma possibly depression
in oxford as in many other uk centers
we've set up a multidisciplinary clinic
um and this seas started off seeing
people had been admitted to hospital but
under pressure from primary care
it now sees in fact the majority of
patients are referrals from primary care
as you can see consistent with the nice
recommendation it has a range of
disciplines
in a one-stop shop multi-disciplinary
clinic
and we also have a virtual
multi-disciplinary team where we can
bring in cardiology neurology and so on
when needed
this has been a very interesting
development i think this is how medicine
should be practiced
but of course it's on short-term funding
um and long-term funding is promised but
who knows so let's start with a case
um there's a range of types of people
and symptoms but if it was to be a
common case
that would be a gp referral and most of
the
the more curiously the more complex
patients tend to be the gp referrals not
the hospital discharges
a woman in her 30s 40 uh
teacher small children had a coveted
like illness about six months ago
wasn't tested so we have to take it on
the symptoms
and is now presenting to the clinic with
disabling fatigue
that she says is made worse when she
does things widespread aches and pains
short of breath and feeling of heaviness
in the chest
and generally very anxious about her
illness and about what's going to happen
and has not been back to work since the
um since she became ill so there's a
wide range of presentations but this
would be a common type of presentation
and as you'll see the symptoms that she
presents are the same as the ones
that come out in surveys so chest pain
shortness of breath
sometimes cough aches and pains and the
most common
and often most disabling symptom fatigue
the other thing you'll notice from this
diagram is there are a lot of symptoms
and i should say that's a short list
compared to some of the things you'll
see if you look on the web
so we're dealing with a large number of
symptoms with certain ones
core to this presentation i think
importantly for our talk today
it's not just symptoms it's function and
particularly
work uh this is data just from a hundred
patients
seen in the postcode clinics in oxford
and cardiff
and as you'll see more than half are not
back at full time work
six months after infection and a quarter
have not gone back to work at all
um this is mainly hospitalized patients
so in the non-hospitalized patients the
figures may even be higher
so so that's the that's the the
presentation
that we're dealing with what do we know
about the causes
and my takeaway message for causes is
that
it's very easy to find oneself talking
about postcovid syndrome as if it's a
thing like lung cancer
and i don't think it's just the
presentations so we must allow for the
fact that it'll be heterogeneous
and we must be very wary about thinking
about a single cause
and in fact the clinical experiences the
causation
is complex so i'm just going to run
through
potential causal factors um
on the basis of our clinical experience
um
as biological psychological and social
so the thing that everyone thinks about
is organ damage
and clearly there is frequently some
damage to lungs
our experience is that tends not to
progress and usually tends to resolve
people do have acute abnormalities in
kidneys heart
possibly brain um but again what we're
finding is to follow up
the relevance of these abnormalities to
people's presentation
is often unclear and often there isn't
very much in the way of investigation
abnormalities
people hypothesize that some resetting
of immune function
that remains a hypothesis it's not
apparent on normal testing
patients often complain of tachycardia
or postural blood pressure drops
and that's um referred to as autonomic
dysfunction i don't think anyone really
understands that
i think it's largely assumed to be
something that will be reversible but
it's a physiological abnormality
and then of course um this is often been
a serious illness
and as the consequence is the way people
have coped with it so if they've gone
from being
running marathons to lying in bed that's
going to have profound effects on their
physiology and their muscle mass
some people become very preoccupied with
their breathing very anxious with their
breathing
maybe over breathe and that of course
can produce
biochemical changes and make people feel
unwell
so there are a range of biological
factors
and the the specific evidence of organ
damage
is present in some people but it is not
the majority
at least not the majority is the cause
of the symptoms
and one of the things i see written a
lot i wanted to
take away message is these people have a
lot of symptoms often
may have 20 30 symptoms multi-symptom
illness does not mean multi-system
pathologies people talk about systems
related to the
heart the lung the brain and that
doesn't mean that those organs are all
diseased it just means the patient
has multiple symptoms
so let's move on to the psychological
factors and what's very striking in some
of our patients
is what you might call health anxiety
they're very focused on bodily symptoms
uh they're worried understandably what
they might mean
particularly focused on breathing and
experience of being breathless
anxiety is prevalent in this population
a third to a half of patients have
significant anxiety
and because of that fearfulness they may
avoid going out and they may spend a lot
of time seeking information
about their condition because it's known
to be a little mysterious
and they may seek a lot of medical care
and we'll come back to that
i think i my colleagues think that
social factors
have an influence in shaping these
presentations and the concern about
symptoms
so here's an article by a well-known
journalist in a well-known newspaper
and as you can see he says that uh
long cove could mean lifelong coping the
effects can be horrible
there's damage in the lung heart and
brain and we should all fear lasting
consequences
so if you're a somewhat vulnerable
disposition and you're feeling unwell
and you don't know much about your
illness that is likely to make you more
concerned
and is not conducive to a positive
approach to recovery and inevitably as a
feature of the modern world
there are a lot of online groups being
even more important in this pandemic
um great benefit to many patients who
feel worried about their symptoms and
feel maybe they're the only one to be
able to share those experiences and get
some support
potentially downside as we've seen with
the chronic fatigue and me groups
who are also moving into this space to
some degree is the people that recover
tend to leave
and you end up over time with the poor
prognosis people
who have a rather pessimistic view of
the illness that they transfer to other
people
so i'm not sure that all the support
groups have been entirely helpful
in encouraging the patient to take a
positive approach
and of course our old friends doctors
are sometimes unhelpful here this is a
quotation from an immunologist
that was reported in nature um
their physicians don't believe them and
so they get psych referrals
so you know it's not really real you're
sent to psychiatry
and his mission is to tell the people i
have a real disease
and what's causing it and of course
that's an another
noble mission but it can lead to
excessive investigation
often an investigation in multiple
species over a period of time
which isn't necessarily helpful to the
patient
and indeed can entrench the patient in
worries
that they have a disease and again
distract them from the task
of rehabilitation so
we don't know the causes so please uh
accept that what i've said is based on
uh clinical experience and a smattering
of evidence
but we think probably certainly for the
primary care patients
by a psychosocial perspective these
different factors
interplaying in different ways is gets
more and more relevant as the patient's
illness and disability
gets more chronic
so we're dealing with a heterogeneous
and complex syndrome what do we know
about
treatment and and here another takeaway
message
in working in the clinic is some of my
colleagues feel that they need to keep a
completely open mind on this condition
it's a new illness
anything could be going on so they need
to do as many tests as possible
whereas the opposing approach is
actually
we don't know but most of this looks
pretty familiar this is anxiety it's
chronic fatigue
we know how to treat those we know about
rehabilitation let's just be pragmatic
and i think one of the real challenges
for managing this condition is
somehow to keep that balance and not to
go too far and over investigation and
not to get too complacent that we know
what's going on
it's a challenge
Esther12
Senior Member (Voting Rights)
part 2:
so the basic management
that
we would do in the clinic and this is
good
management for anything really is that
the patients often come to the clinic as
they do with these kinds of illness
feeling uh not believed feeling that
maybe people are accusing them of making
up their symptoms no one's really taken
an interest
and so spending some time listening to
and showing you uh believe their
experience is really
first base and if you don't do that you
it's hard to get much further to be
honest so that's a crucial starting
point
i think the physicians have to manage
the patient's uncertainty and their own
uncertainty
in deciding how many avenues to go down
with possibilities and tests
and how much to be pragmatic
we must remember it's heterogeneous and
we do find treatable conditions
um about 10 percent have major
depression
uh a significant number have new onset
or exacerbation of asthma
we occasionally find hypothyroidism so
there are simple
things to treat that one can find and
treat
i think what's really important is that
as far as we know most people improve
and so
to give an overall positive message
rather than this is a very worrying
alarming condition that we don't
understand and we don't know what's
going to happen to you
and then the approach for most people is
a
gentle slow return to activity
and at this point some of you uh will be
noticing there are some similarities
here with
approaches to many other illnesses
chronic fatigue syndrome
post line post head minor head injury
all these things
um and indeed there are and it's
tempting to see
kovid as chronic fatigue syndrome with a
cough
but i think that's a little bit
dangerous to make just facile
comparisons but there certainly are some
similarities
and so we don't have any randomized
trials of treatment and postcoded yet
because we haven't had time to have them
done but we have got randomized
trials in these related conditions so
this is the trial
that uh i did with colleagues about 10
years ago
in chronic fatigue syndrome and
basically different treatments were
tested you can see here smc
standard medical care gets graded
exercise
apt is pacing living within your limits
and cbt
cbt so basically they fall into the
the rehabilitative treatments those that
encourage
people with care to gradually build on
what they can do and not worry too much
about the consequences of that
that's the bottom two and the top two
are the ones the more conservative ones
just medical care
or live within your limits and you could
see there at 52 weeks in this
trial there was a clear greater
reduction in fatigue
perhaps paradoxically of those that had
the more active rehabilitation
and similar greater physical
function in those that had the more
active rehabilitation
and this idea of just pacing just
accepting your limits
is no better and possibly actually
slightly worse than nothing
than medical care so that has been
again some you may know immensely
controversial
because uh some of the patient groups
are very against this they feel it's um
it's harmful it's uh not validating
their illness
and so that leads to some potential
difficulties
for us in helping patients but i think
at the moment
if you've found and treated the obvious
things you can treat
the best approach to pros covid is
accepting it'll take time
and doing what i might call
psychologically informed robot
rehabilitation explicitly dealing with
worries
but helping them very gently return to
activity
so if rehabilitation is at the moment
our best hope what are the challenges in
providing that to our patients
well the obvious challenge is there
aren't many rehabilitation
multi-disciplinary teams as you could
see a picture of there
they're being set up certainly in some
places in the uk
with short-term funding um as we have in
oxford but
it's patchy the national health service
in the uk
isn't generally good it's good as acute
illness it's not quite so good at
rehabilitation
and the complicating factor is that nice
who is the authority that
that recommends treatments is
potentially in a contrary position
they've done provisional guidelines on
the management of post covid
which are good guidelines uh i think
that they're they're not very specific
but they're very sound
but they're also doing guidelines on
any chronic fatigue syndrome which in
their current form
they're being revised in in the light of
feedback
are say you shouldn't have
rehabilitation and graded exercise
so i don't know how that's going to play
out but that may complicate the
provision of treatment
for postcovid patients
so what you really want to know is
okay there's all this stuff it's very
complicated and we rehabilitate
how well are people going to do how many
going to end up
from the swiss re perspective of having
chronic disability and chronic work
disability
and that's the one thing of course we
don't know because it hasn't been around
long enough
but i think our experiences to date
that most patients do do improve um
it may be slow we may be talking months
rather than weeks
but with some advice a bit of follow-up
most people do improve
so as far as we can see that approach of
getting people to have a sound
understanding
and not worry too much and work on
rehabilitation is helpful
in the absence of really good data um
physicians usually fall back as you know
on the rule of thirds
so my guess would be about a third these
people won't do so well
about a third will do very well and
about a third will be somewhere between
the two
and so if we say we've got five percent
and we
applies the rule of thirds a guess would
be
someone something like one percent of
these people may have some long-term
disability
uh that is a guess and it'll depend on
the care people get
but given the number of people with
covid that could potentially be quite a
lot of people
sorry nice slides there we go so i want
to provide another case study this is an
unusual case study because um
this one is in the public domain this is
paul garner who's a professor of
medicine
university of liverpool and he's
actually
blogged in the bmj uh
his initial onset
of long covered and now his recovery
and it it's probably worth reading so he
had a
kobe like illness he was very
symptomatic and disabled he couldn't
work
he describes it very well and then he
actually
he was becoming to believe he had me a
chronic possibly lifelong illness and
then he had contact with someone
expert in rehabilitation of chronic
fatigue syndrome and he recovered
quite quickly with a different approach
of rehabilitation
so we don't want to argue too far from
single cases
but it's such a high profile example
it's quite interesting and one you can
read about
oops so um
apologies for that so just to summarize
um those are my take-home messages
beware of the poor quality research
don't assume post-covet is a thing just
because they've got a lot of symptoms
doesn't necessarily mean there's a lot
wrong with them
um we need this open mind of balancing
it could be all sorts of things with we
need to be pragmatic
there are similarities with other
illnesses like chronic fatigue syndrome
probably the best treatment is
psychologically informed rehabilitation
at the moment that may change and
from the insurers point of view i
suspect there is likely to be long-term
disability
and the precise numbers and severity i'm
afraid remains to be seen
those are three things that are probably
worth looking at the nice guidance
um there's a very recent sensible paper
from a respiratory clinic by
sykes in lung and paul garner's essays
in the bmj for a patient perspective
thank you very much
thank you professor sharp that's
incredibly helpful
we have lots of questions as you uh you
might imagine
um so i'll start going through some of
those one question
i had actually was whether you noticed
any marked differences in the kind of
patients that you saw that rooted from
being followed up after discharge from
admissions with covid
versus the referrals that you had from
the community
um yes that may change over time
um but quite a striking difference
the patients will be in hospital tend to
be
older and even even elderly at their
follow-up
three months um they often have some
respiratory symptoms
they may have had some deconditioning
they're being in itu
but they're relatively simple that's
what they've got
the ones we're getting from primary care
these are averages on average and much
more complicated with much more anxiety
depression complex backgrounds mixed in
so that may just be an artifact of
current referral patterns
and it may be the ones that seem most
complex the gps are referring
and we'll see how it evolves over time
but it has been a striking
observation in the clinic yes
interesting um
another question we had was around um
determining the veracity of reported
symptoms
so you have this issue of of belief
having an impact on on prognosis
versus kind of whether any there's any
manipulation of
of symptoms what's your experience of
that
well that's a complex area isn't it and
it applies to all of medicine
i think one's more likely to see that
whether whatever the illness if people
stand to gain or lose
on an insurance policy or whatever
leaving the army or whatever
i think at this stage in the game at the
relatively early stage
i think people's if there is an excess
symptom presentation
it's driven more by fear and anxiety by
and possibly attempt possibly to
convince the doctors but mainly by fear
and anxiety
rather than any attempt to manipulate i
think as any illness as you know any
illness gets chronic
and people stand to gain a large payout
whatever then people
may obviously emphasize their symptoms
we're not seeing that at the moment
and thank you and another question um
from the floor is is regarding um the
impact of the
long covered clinic work on
re-hospitalization
do you have any feel for whether it's
managed to reduce that or whether
whether it's a separate issue
um well in in oxford thankfully we
we didn't have a massive we had a
moderate number we didn't have a massive
number of hospitalized cases
uh and the majority of people now been
seen in our clinic uh primary care
referrals it's hard to know
one of the things we have found that
we're trying to do with the
clinic is prevent the multiple referrals
so when i was saying
that people get referred to multiple
specialties that isn't just within the
clinic
people are rattling around the hospital
as you can imagine from cardiology to
neurology to rheumatology
and i think one benefit of having a post
kobe clinic is you can try and pull them
in
and keep a handle on that and so you
know we have a cardiologist we'll
join virtually in our mdt but the
patients don't all have to go to
cardiology
so i think we are containing the
healthcare use and hopefully the adverse
effects of all those opinions on the
patient
excellent thank you um one question um
was regarding whether there are any
imaging studies that might link to
factors in in the the fatigue elements
of of long covered or wider are you
aware of any
any imaging studies on that topic do you
know if we
go into the literature on chronic
fatigue syndrome and other fatigue
states there are thousands
of studies of all sorts of things and
there certainly are imaging studies um
i don't i'm not aware of anything that's
giving us a generally accepted answer in
either condition
but whatever your hypothesis you will
find a a study
and some of those may turn out to be
right but at the moment but they're not
accepted the main
the main imaging abnormalities are just
um chest x-ray and chest ct
where you generally see resolving
fibrosis and that's
that's the main abnormalities that we
see
one last question before we move on to
our next speaker is um
regarding the the change in the the nice
guidelines um and i'm wondering whether
that has any impact on
our ability to to manage this this
patient group
gosh well that's an interesting uh
highly political
moving uh target there um
the nice guidance existing nice gardens
for chronic fatigue syndrome
me advocated rehabilitation in the form
of cbt graduate exercise
the revision of the guidance which has
been very driven by
by patient groups who feel strongly
about this
is going was going to be very different
that's been out to consultation
i know several royal colleges have
pushed back very hard indeed on that
and it's being considered and that will
come out in march
on the positive side at the moment the
postcovid nice guidance
is very very sensible very pragmatic and
advocates rehabilitation so i think
there's lots to play out there
what will happen with the chronic
fatigue me once what will happen with
the nice ones
but you know i think we just have to we
just have to have this rehabilitation
because it's the only thing we've got
apart from time
absolutely that's that's wonderful thank
you so much for taking the time to speak
to us today that's very kind of you
thank you
great pleasure thank you very much
Sharpe lists support groups as one of the "social factors" that influence recovery -- included are Long Covid Support and ME Action's "Long Covid and ME - Understanding the connection" group.
He says that "At present the best treatment is psychologically informed rehabilitation", accompanied by slides showing improvement from GET and CBT in the PACE trial. Meanwhile, he puts the NICE ME/CFS draft guidelines under "Challenges in providing rehabilitation".
Admittedly, I didn't expect he would tell Paul Garner's story as a "Case study from the BMJ". But he did.
Trying to remember the paper where I first read this, I think it Wessley or White, but it was an older paper that highlighted financial gain (e.g. from disability) as well.
edit: So far, couldn't find the paper I was looking for, although this one (1992) by Sharpe. My bolding.
Functional impairment was significantly associated with belief in a viral cause of the illness (odds ratio = 3.9; 95% confidence interval 1.5 to 9.9), limiting exercise (3.2; 1.5 to 6.6), avoiding alcohol (4.5; 1.8 to 11.3), changing or leaving employment (3.1; 1.4 to 6.9), belonging to a self help organization (7.8; 2.5 to 23.9), and current emotional disorder (4.4; 2.0 to 9.3).
Alternatively, they may indicate factors that tend to maintain functional impairment. Thus membership of a patient organisation may be an understandable consequence of a more disabling illness or, alternatively, could be a marker of beliefs in physical causation and the need to limit activity which may perpetuate illness.
Telling, conclusion in Sharpe's own words, I wonder, if he is present the conclusion that support groups are dangerous, and his own conclusions are uncertain and opposite, that maybe did he mention both sides in the presentation or present evidence for his conclusion? As the paper above provides no evidence that they are a perpetuating factor.
Last edited:
Esther12
Senior Member (Voting Rights)
Just a couple of excerpts from Sharpe.
On PACE:
On Long Covid rehab:
On PACE:
this is the trial
that uh i did with colleagues about 10
years ago
in chronic fatigue syndrome and
basically different treatments were
tested you can see here smc
standard medical care gets graded
exercise
apt is pacing living within your limits
and cbt
cbt so basically they fall into the
the rehabilitative treatments those that
encourage
people with care to gradually build on
what they can do and not worry too much
about the consequences of that
that's the bottom two and the top two
are the ones the more conservative ones
just medical care
or live within your limits and you could
see there at 52 weeks in this
trial there was a clear greater
reduction in fatigue
perhaps paradoxically of those that had
the more active rehabilitation
and similar greater physical
function in those that had the more
active rehabilitation
and this idea of just pacing just
accepting your limits
is no better and possibly actually
slightly worse than nothing
than medical care so that has been
again some you may know immensely
controversial
because uh some of the patient groups
are very against this they feel it's um
it's harmful it's uh not validating
their illness
and so that leads to some potential
difficulties
for us in helping patients but i think
at the moment
if you've found and treated the obvious
things you can treat
the best approach to pros covid is
accepting it'll take time
and doing what i might call
psychologically informed robot
rehabilitation explicitly dealing with
worries
but helping them very gently return to
activity
so if rehabilitation is at the moment
our best hope what are the challenges in
providing that to our patients
well the obvious challenge is there
aren't many rehabilitation
multi-disciplinary teams as you could
see a picture of there
they're being set up certainly in some
places in the uk
with short-term funding um as we have in
oxford
On Long Covid rehab:
the complicating factor is that nice
who is the authority that
that recommends treatments is
potentially in a contrary position
they've done provisional guidelines on
the management of post covid
which are good guidelines uh i think
that they're they're not very specific
but they're very sound
but they're also doing guidelines on
any chronic fatigue syndrome which in
their current form
they're being revised in in the light of
feedback
are say you shouldn't have
rehabilitation and graded exercise
so i don't know how that's going to play
out but that may complicate the
provision of treatment
for postcovid patients
so what you really want to know is
okay there's all this stuff it's very
complicated and we rehabilitate
how well are people going to do how many
going to end up
from the swiss re perspective of having
chronic disability and chronic work
disability
and that's the one thing of course we
don't know because it hasn't been around
long enough
but i think our experiences to date
that most patients do do improve um
it may be slow we may be talking months
rather than weeks
but with some advice a bit of follow-up
most people do improve
so as far as we can see that approach of
getting people to have a sound
understanding
and not worry too much and work on
rehabilitation is helpful
in the absence of really good data um
physicians usually fall back as you know
on the rule of thirds
so my guess would be about a third these
people won't do so well
about a third will do very well and
about a third will be somewhere between
the two
and so if we say we've got five percent
and we
applies the rule of thirds a guess would
be
someone something like one percent of
these people may have some long-term
disability
uh that is a guess and it'll depend on
the care people get
but given the number of people with
covid that could potentially be quite a
lot of people
