Dolphin
Senior Member (Voting Rights)
https://www.sciencedirect.com/science/article/abs/pii/S0022399919306555
https://doi.org/10.1016/j.jpsychores.2020.110133
Journal of Psychosomatic Research
Available online 5 May 2020, 110133
In Press, Journal Pre-proofWhat are Journal Pre-proof articles?
The role of partners' fatigue and the patient-partner relationship in the outcome of cognitive behavioural therapy for chronic fatigue syndrome
Annemarie Braamse(a), Hille Voss(b), Stephanie Nikolaus(b), Alison
Wearden(c), Hans Knoop(a,b)
a
Department of Medical Psychology, Amsterdam University Medical Centers, University of Amsterdam, Amsterdam, the Netherlands
b
Expert Center for Chronic Fatigue, Department of Medical Psychology, Amsterdam University Medical Centers, VU University, Amsterdam, the Netherlands
c
School of Health Sciences, University of Manchester, Manchester, United Kingdom
Received 19 July 2019, Revised 4 May 2020, Available online 5 May 2020.
https://doi.org/10.1016/j.jpsychores.2020.110133
Highlights
•
Partners of patients with chronic fatigue syndrome have lower fatigue than controls.
•
Fatigue in partners is not related to chronic fatigue patients' fatigue.
•
Higher fatigue severity in female partners predicts worse CBT outcome for patients.
•
Female partners' relationship dissatisfaction predicts worse CBT outcome for patients.
Abstract
Background
In chronic fatigue syndrome (CFS) little is known about how partner-related factors influence patients' fatigue symptoms and treatment outcome. We examined partners' fatigue severity, and determined the role of partner-related factors for patients' symptoms and the outcome of cognitive behavioural therapy (CBT).
Methods
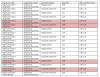
1356 CFS patients and their partners completed baseline measures of fatigue severity (Checklist Individual Strength), causal attributions of symptoms, partner responses to patient symptoms, and relationship satisfaction. Fatigue in partners of patients with CFS was compared with fatigue in age- and gender-matched controls from the Dutch population. Associations between partners' fatigue severity and other partner-related factors were determined. In a subgroup of 760 CFS patients who completed CBT, logistic regression analyses were used to identify partner-related baseline predictors for treatment outcome (fatigue severity, functional impairment).
Results
Partners' fatigue (M = 21.66, SD 11.60) was significantly lower than in controls (M = 24.58, SD = 11.02) (p < .001) and not related to patients' fatigue (r = −0.02, p = .58). Partners' fatigue was correlated with patients' functional impairment (p = .001), partners' and patients' relationship dissatisfaction, negative partner responses, and partners' and patients' psychological attributions of patient symptoms at baseline (all p < .001). After controlling for patients' baseline fatigue severity and functional impairment, only relationship dissatisfaction as reported by (female) patients significantly predicted worse treatment outcome. For male patients with female partners, higher partners' fatigue severity predicted higher fatigue severity after CBT.
Conclusions
Female partners' fatigue and relationship dissatisfaction as reported by the female patient should be addressed in CBT for CFS, as these factors affect treatment outcome.
Keywords
Chronic fatigue syndrome
Cognitive behavioural therapy
Patient-partner relationship
Partners' fatigue severity
Partners' responses
Treatment outcome