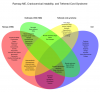
If helpful, here is a DRAFT Venn diagram of symptoms from awhile back. I catalogued symptoms mentioned by Ramsay in his 1990s paper, symptoms reported in the outbreaks literature (I think it had to be mentioned in at least two papers but I forget what criteria I used), along with tethered cord symptoms and CCI symptoms. There may be some errors an omissions of course, but I tried to take great care.
I have done the same with CCC and ICC diagnostic criteria, if that is of interest to anyone.
You can see that there is in fact some overlap.
If patients with CCI and tethered cord are being misdiagnosed with ME, you could see why this could happen if the clearer signs of nerve compression were dismissed or if the patient never reported them. In the beginning, I went to every doctor with a list of 40 symptoms. It was a very challenging clinical picture to tease out, in particular because I had THREE pathologies at once: CCI, tethered cord and MCAS. (I believe MCAS interacts with CCI and tethered cord in some ways we don't yet understand and there is some literature on this, or at least, MCAS + spinal injuries.)
The sadness of all this is that when my neurologist in 2012 (the one who diagnosed me with conversion disorder) asked me to walk, he saw the problems I had with my gait and thought they were hysterical. If he had simply asked me to walk on my heels and toes, it would have been clear I had a tethered spinal cord and things might have happened very differently for me and others like me.
It is also important to note that patients on FB are getting diagnosed with more than CCI/AAI. They have Chiari, *surgical* cervical stenosis, tethered cord syndrome, Eagle's Syndrome, Klippel-Feil syndrome, scoliosis, etc. A lot of missed diagnoses. There is a lot of overlap between these conditions and connective tissue disorders. I'm perfectly happy to view this as a nosological problem, where even the most "strict" definitions are preventing people from getting the investigation they need and deserve.
I have done the same with CCC and ICC diagnostic criteria, if that is of interest to anyone.
You can see that there is in fact some overlap.
If patients with CCI and tethered cord are being misdiagnosed with ME, you could see why this could happen if the clearer signs of nerve compression were dismissed or if the patient never reported them. In the beginning, I went to every doctor with a list of 40 symptoms. It was a very challenging clinical picture to tease out, in particular because I had THREE pathologies at once: CCI, tethered cord and MCAS. (I believe MCAS interacts with CCI and tethered cord in some ways we don't yet understand and there is some literature on this, or at least, MCAS + spinal injuries.)
The sadness of all this is that when my neurologist in 2012 (the one who diagnosed me with conversion disorder) asked me to walk, he saw the problems I had with my gait and thought they were hysterical. If he had simply asked me to walk on my heels and toes, it would have been clear I had a tethered spinal cord and things might have happened very differently for me and others like me.
It is also important to note that patients on FB are getting diagnosed with more than CCI/AAI. They have Chiari, *surgical* cervical stenosis, tethered cord syndrome, Eagle's Syndrome, Klippel-Feil syndrome, scoliosis, etc. A lot of missed diagnoses. There is a lot of overlap between these conditions and connective tissue disorders. I'm perfectly happy to view this as a nosological problem, where even the most "strict" definitions are preventing people from getting the investigation they need and deserve.